In the emergency department, troponin determination is a useful test to differentiate between non–ST-segment myocardial infarction (MI) and unstable angina. Acute and chronic myocardial lesions due to a large spectrum of cardiac and noncardiac causes are recognizable in clinical practice.1 In 2007, the universal definition of MI established the classification of patients according to the etiology of the condition.2 Since then, the term type 2 MI has been used to describe clinical conditions associated with an ischemic myocardial lesion in the absence of complicated atheromatous plaques. Although several studies have reported higher mortality rates in patients with type 2 MI than in those with type 1, discrepancies remain regarding this prognosis, possibly because of the different diagnostic criteria used.3–5 Nonetheless, there are no studies investigating the degree of acceptance of this classification or the extension of its use in clinical practice. Our aim was to evaluate the concordance between diagnosis associated with a troponin elevation in medical reports and diagnosis according to the universal definition of MI in patients with a positive troponin result and no acute coronary syndrome (ACS).
A retrospective study was carried out in a university hospital, including all consecutive patients admitted to the emergency department between January 2012 and December 2013 with at least 1 troponin determination. The exclusion criteria were as follows: troponin determination lower than the 99th percentile reference value, age younger than 18 years, patient recovering from cardiac arrest, patient with myocarditis, residence outside the hospital catchment area, and type 1 MI. Troponin determinations were all performed using the same immunoassay (Siemens Advia Centaur troponin I-Ultra; 99th percentile reference value 0.039 ng/mL and coefficient of variation < 10%). The diagnoses were categorized by consensus between 2 cardiologists: a) type 2 MI was established based on the criteria of Saaby et al.6 (who used a contemporary troponin assay having greater analytical imprecision than that used in our study), and b) myocardial injury without an ACS: patients with high troponin values who did not meet the criteria for type 2 MI. The study was approved by the local ethics committee. Patients were divided into 4 groups according to the department discharging them (cardiology, internal medicine, emergency, and others). The diagnoses associated with the troponin elevation in the discharge reports were classified into 5 categories: type 2 MI, myocardial injury without an SCA, secondary SCA, not specified, and others.
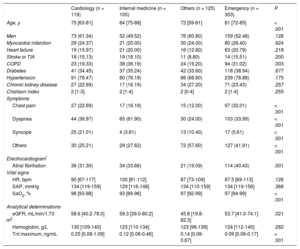
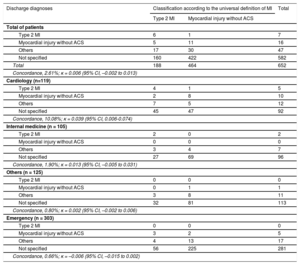
In total, 652 patients were included in the analysis. Baseline characteristics are shown in Table 1. Patients hospitalized in internal medicine had a history of chronic obstructive pulmonary disease more often. Dyspnea was the main symptom in patients hospitalized in cardiology and internal medicine, whereas atypical symptoms were more common in those hospitalized in other departments and in patients directly discharged from the emergency department. Of the 188 patients categorized as having type 2 MI, the discharge reports specified this diagnosis in only 6 patients (3.2%); of the 464 patients with myocardial injury, the discharge reports specified this diagnosis in only 11 (2.4%). The overall concordance between the categorization and the diagnosis recorded in the discharge reports was 2.61% (κ = 0.006; 95% confidence interval, –0.002 to 0.013). The results of the overall analysis and the analyses according to the department issuing the discharge report are shown in Table 2.
Patients’ Baseline Clinical Characteristics of the Patients According to the Department Issuing the Discharge Report
| Cardiology (n = 119) | Internal medicine (n = 105) | Others (n = 125) | Emergency (n = 303) | P | |
|---|---|---|---|---|---|
| Age, y | 75 [63-81] | 84 [75-88] | 72 [59-81] | 81 [72-85] | < .001 |
| Men | 73 (61.34) | 52 (49.52) | 76 (60.80) | 159 (52.48) | .128 |
| Myocardial infarction | 29 (24.37) | 21 (20.00) | 30 (24.00) | 80 (26.40) | .624 |
| Heart failure | 19 (15.97) | 21 (20.00) | 16 (12.80) | 63 (20.79) | .218 |
| Stroke or TIA | 18 (15.13) | 19 (18.10) | 11 (8.80) | 14 (15.51) | .200 |
| COPD | 23 (19.33) | 38 (36.19) | 24 (19.20) | 94 (31.02) | .003 |
| Diabetes | 41 (34.45) | 37 (35.24) | 42 (33.60) | 118 (38.94) | .677 |
| Hypertension | 91 (76.47) | 80 (76.19) | 86 (68.80) | 239 (78.88) | .175 |
| Chronic kidney disease | 27 (22.69) | 17 (16.19) | 34 (27.20) | 71 (23.43) | .257 |
| Charlson index | 2 [1-3] | 2 [1-4] | 2 [0-4] | 2 [1-4] | .255 |
| Symptoms | |||||
| Chest pain | 27 (22.69) | 17 (16.19) | 15 (12.00) | 97 (32.01) | < .001 |
| Dyspnea | 44 (36.97) | 65 (61.90) | 30 (24.00) | 103 (33.99) | < .001 |
| Syncope | 25 (21.01) | 4 (3.81) | 13 (10.40) | 17 (5.61) | < .001 |
| Others | 30 (25.21) | 29 (27.62) | 72 (57.60) | 127 (41.91) | < .001 |
| Electrocardiogram* | |||||
| Atrial fibrillation | 36 (31.30) | 34 (33.66) | 21 (19.09) | 114 (40.43) | .001 |
| Vital signs | |||||
| HR, bpm | 90 [67-117] | 100 [81-112] | 87 [73-109] | 87.5 [69-113] | .126 |
| SAP, mmHg | 134 [119-159] | 129 [116-148] | 134 [110-159] | 134 [119-156] | .368 |
| SaO2, % | 96 [93-98] | 93 [89-96] | 97 [92-99] | 97 [94-99] | < .001 |
| Analytical determinations | |||||
| eGFR, mL/min/1.73 m2 | 58.6 [40.2-78.0] | 59.3 [39.0-80.2] | 45.8 [19.8-82.3] | 53.7 [41.0-74.1] | .021 |
| Hemoglobin, g/L | 130 [109-140] | 123 [110-134] | 123 [98-139] | 124 [112-140] | .282 |
| TnI maximum, ng/mL | 0.25 [0.08-1.09] | 0.12 [0.06-0.46] | 0.14 [0.08-0.67] | 0.09 [0.06-0.17] | < .001 |
COPD chronic obstructive pulmonary disease; eGFR, estimated glomerular filtration rate; HR, heart rate; SAP, systolic arterial pressure; SaO2, arterial oxygen saturation; TIA, transient ischemic attack; TnI, troponin I
The data are expressed as No. (%) or median [interquartile range].
Analysis of Concordance Between the Diagnoses in the Discharge Reports and the Classification According to the Universal Definition of MI in the Overall Sample and by the Department Issuing the Report
| Discharge diagnoses | Classification according to the universal definition of MI | Total | |
|---|---|---|---|
| Type 2 MI | Myocardial injury without ACS | ||
| Total of patients | |||
| Type 2 MI | 6 | 1 | 7 |
| Myocardial injury without ACS | 5 | 11 | 16 |
| Others | 17 | 30 | 47 |
| Not specified | 160 | 422 | 582 |
| Total | 188 | 464 | 652 |
| Concordance, 2.61%; κ = 0.006 (95% CI, –0.002 to 0.013) | |||
| Cardiology (n=119) | |||
| Type 2 MI | 4 | 1 | 5 |
| Myocardial injury without ACS | 2 | 8 | 10 |
| Others | 7 | 5 | 12 |
| Not specified | 45 | 47 | 92 |
| Concordance, 10.08%; κ = 0.039 (95% CI, 0.006-0.074) | |||
| Internal medicine (n = 105) | |||
| Type 2 MI | 2 | 0 | 2 |
| Myocardial injury without ACS | 0 | 0 | 0 |
| Others | 3 | 4 | 7 |
| Not specified | 27 | 69 | 96 |
| Concordance, 1.90%; κ = 0.013 (95% CI, –0.005 to 0.031) | |||
| Others (n = 125) | |||
| Type 2 MI | 0 | 0 | 0 |
| Myocardial injury without ACS | 0 | 1 | 1 |
| Others | 3 | 8 | 11 |
| Not specified | 32 | 81 | 113 |
| Concordance, 0.80%; κ = 0.002 (95% CI, –0.002 to 0.006) | |||
| Emergency (n = 303) | |||
| Type 2 MI | 0 | 0 | 0 |
| Myocardial injury without ACS | 3 | 2 | 5 |
| Others | 4 | 13 | 17 |
| Not specified | 56 | 225 | 281 |
| Concordance, 0.66%; κ = –0.006 (95% CI, –0.015 to 0.002) | |||
95% CI, 95% confidence interval; ACS, acute coronary syndrome; MI, myocardial infarction
Our study performed in daily practice shows that a number of patients in the emergency department with a wide variety of clinical diagnoses have elevated troponin values. In these patients, diagnosis related to troponin elevation is specified in very few discharge reports, which indicates that acceptance of the terms type 2 MI and myocardial injury is lacking. In some cases, clinicians hesitate to assign a diagnosis of type 2 MI and, in contrast, “accept” a diagnosis of myocardial injury. There are several possible reasons for this finding. Physicians may avoid classifying patients as having type 2 MI or myocardial injury because of uncertainty that there is an underlying coronary disease. Or they may wish to avert treatments when there is scientific evidence of type 1 MI, but insufficient evidence to support treatment in the absence of a complicated atherothrombotic plaque. Another possible explanation is a lack of understanding of what actually constitutes type 2 MI. For type 2 MI and myocardial injury to be universally accepted, there should be broad consensus on the criteria to establish these diagnoses. This would enable standardization of research and identification of therapeutic strategies that could modify the prognosis. Perhaps when the evidence reaches this point, clinical acceptance of the terms included in the universal definition of MI will become more widely recognized. This study has the limitations of a single-center design and inclusion of patients with only 1 troponin determination, factors that may have had an impact on assigning some of the diagnoses.
.