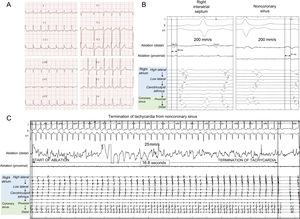
A 77-year-old woman with severe rheumatic aortic stenosis and paroxysmal atrial fibrillation was admitted for aortic valve replacement. After the surgery (21-mm Perceval S sutureless aortic bioprosthesis [Sorin Group] and isolation of pulmonary veins with bipolar radiofrequency ablation forceps), the patient was moved to the postoperative surgical intensive care unit. Two days later, she developed repeated runs of atrial tachycardia (AT) (Figure 1A) with hemodynamic compromise. The tachycardia was refractory to treatment with amiodarone and atenolol, so urgent ablation was performed.
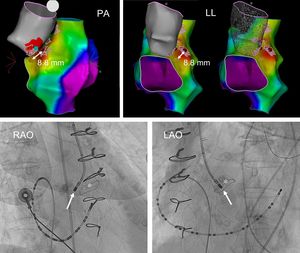
A 24-pole catheter (Orbiter, Bard Medical) was positioned around the tricuspid ring with the distal portion in the coronary sinus. The patient was showing spontaneous runs of narrow-complex tachycardia, with 1:1 A:V conduction, alternating with Wenckebach phenomenon with a constant A-A interval and variable V-A interval, allowing confirmation of the diagnosis of AT. The earliest atrial electrogram on the 24-pole catheter was found in the coronary sinus ostium. An electroanatomic map of the right atrium was created (Carto navigation system, ThermoCool irrigated ablation catheter, SmartTouch J curve for mapping; Biosense, Webster) (Figure 2), on which the earliest atrial electrogram site was in the anterior interatrial septum, 8.8mm posterior to the bundle of His. This distance was considered safe for ablation with radiofrequency (rather than cryoablation). The focal ablation (2 applications; 45 and 65 s, power, 35-40W) suppressed the tachycardia without affecting the PR interval (after 21 and 25seconds, respectively), but with recurrence (with the same cycle length) after a few minutes. An extension was performed superior to the ablation (40 s, 35W), unsuccessfully. Therefore, an electroanatomic map of the aortic root was created, mapping specifically the noncoronary sinus of Valsalva. The presence of the aortic prosthesis did not impede the mapping. The earliest atrial electrogram sites were similar to those found in the right interatrial septum (Figure 1B); the distance between the earliest activation site and the prosthetic aortic valve was considered safe for ablation. Focal ablation (initial application: 45 s, 45-50W, successful; additional adjacent application of 30 s at 50W) led to termination of the tachycardia in 17seconds (Figure 1C), which remained uninducible. The patient was discharged 3 days later, and at 6 months’ follow-up she was arrythmia-free with no antiarrhythmic drugs.
Activation map of the right atrium and the aortic root; the color gradation from red to violet indicates the earliest to latest atrial electrogram sites. Larger red spots: earliest right atrial electrogram; yellow spots: site of the bundle of His; blue circle: effective ablation site from the noncoronary sinus; small red dotted area: ablated tissue. The fluoroscopic image of the effective ablation site in the noncoronary sinus is also shown (arrow), posterior to the bioprosthesis (asterisk). LAO, left anterior oblique projection; LL, left lateral projection; PA, posteroanterior projection; RAO, right anterior oblique projection. This figure is shown in full color only in the electronic version of the article.
ATs that arise from the interatrial septum close to the bundle of His are relatively uncommon.1,2 The anterior portion of the interatrial septum is in close relation to the posterior part of the aortic root, such that these tachycardias can be ablated from the noncoronary sinus of Valsalva (and, less often, from the other sinuses of Valsalva). In fact, their theoretical origin is an embryological remnant of retroaortic nodule tissue,3 an extension of the atrioventricular nodule that is situated below the noncoronary sinus. Ablation from the aortic root has higher success rates (88%-100%) and lower recurrence rates (0%-4%)4–6 than ablation from the right or left interatrial septum, and also avoids the risk of atrioventricular block inherent to peri-Hisian ablation via the atria. Therefore, our group systematically maps the aortic root in cases of AT in which the earliest right atrial activation site is posterior or superior to the bundle of His. The originality of the case presented here lies in the recent implantation of an aortic prosthesis as the possible trigger of the AT, which, to the best of our knowledge, has not been previously described in the literature. Because of this, we attempted ablation from the right atrium before mapping the aortic root. We did not map the left interatrial septum, which we could have considered, given the low efficacy that has been reported on ablation from this location (25%-64%)5,6 and the sufficient distance from the earliest atrial electrogram in the aortic root to the prosthesis, which made the ablation safe (Figure 2).
In our hospital, since 2014, 46 patients have undergone focal AT ablations (Figure of the supplementary material); 11 had AT of peri-Hisian origin and were treated with ablation from the aortic root (all from a noncoronary sinus). These patients had similar acute success rates for ablation (100% vs 91%; P = .431) but fewer recurrences of atrial arrhythmias at follow-up (0% vs 26%; P = .009) than patients with AT of other origins.
CONFLICTS OF INTERESTE. Franco and J. Moreno have received consultancy fees from Biosense Webster.