Approximately 12% of idiopathic left ventricular (LV) arrhythmias (VA) originate from the LV summit: a triangular region of the epicardial LV outflow tract with the apex at the bifurcation between the left anterior descending and left circumflex coronary arteries with its base formed by an arc connecting the first septal perforator branch of the left anterior descending coronary artery with the left circumflex coronary artery. It is transected laterally by the great cardiac vein (GCV) at its junction with the anterior interventricular vein (AIV) into an area accessible to ablation inferiorly and an inaccessible area superiorly. Electrocardiographically, right bundle branch block morphology with inferior rightward axis is typically observed. During recent years, ablation of LV summit VA has received increasing attention in the literature, given its significant frequency and the challenging technical aspects of catheter ablation.1–4
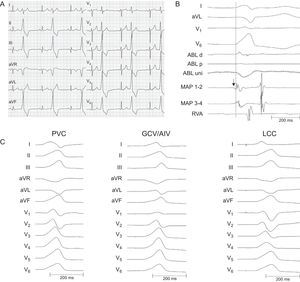
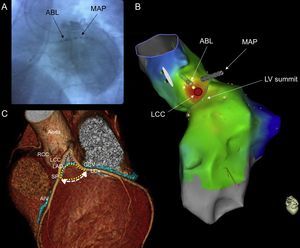
We report the case of a 59-year-old man with a history of ischemic heart disease and normal LV function who presented with palpitations and high density (30%) premature ventricular contractions (PVC) on 24-hour Holter recording. Beta-blockers and amiodarone were ineffective and he was scheduled for an electrophysiologic study that was performed free from antiarrhytmic drugs in a conscious state. The PVC exhibited a QRS complex with a maximum duration of 147ms, right bundle branch block morphology, QRS morphology in V1 and inferior axis of +90° (Figure 1A), suggesting a possible LV summit/outflow origin.1 Mapping and ablation were carried out using a 3.5mm tip irrigated catheter (ThermoCool SF; Biosense Webster) facilitated by an electroanatomic mapping system (CARTO 3). The ablation catheter was first placed in the septal region of the right ventricular outflow tract where poor activation and pace maps were observed. The same catheter was then inserted in the coronary sinus but could only be advanced to the lateral mitral annulus region and consequently it was replaced by a 5 F multipolar catheter, which was successfully advanced out to the GCV/AIV junction. Activation mapping at this site showed a local ventricular signal of 15ms pre-QRS with a near perfect pace mapping (97% concordance). Adjacent structures, such as the aortic-mitral continuity and the left coronary cusp (LCC) and right coronary cusp, were subsequently assessed with the LCC showing the second best activation (0ms pre-QRS) and pace map (91% concordance) (Figure 1B and Figure 1C). Next, a safe distance (> 10mm) between the ablation catheter in the LCC and the left main coronary artery was confirmed by coronary angiography (Figure 2A). Ablation was then carried out in the LCC with power initially set to 30W and maximum temperature to 45°C, aiming for a minimum impedance drop of 10Ω (Figure 2B). Power was eventually titrated up to 50W, which promptly terminated the PVC. During follow-up, the patient showed no further PVC.
A: Twelve-lead electrocardiogram showing PVC; B: Intracardiac electrograms displaying an early fragmented (arrow) signal 15ms pre-QRS on the distal bipole of the MAP catheter located at the GCV/AIV junction. A far-field rounded signal 0ms pre-QRS was recorded on the distal bipole of the ABL catheter positioned at the left coronary cusp; C: Spontaneous PVC and pace-maps at the GCV/AIV junction and LCC with 97% and 92% concordance, respectively. ABL, ablation; AIV, anterior interventricular vein; GCV, great cardiac vein; LCC, left coronary cusp; MAP, mapping; PVC, premature ventricular contractions; RVA, right ventricular apex.
A: Left anterior oblique fluoroscopy view of the ABL catheter positioned at the LCC and the MAP catheter advanced out to the GCV/AIV junction. Coronary angiography revealed a safe distance between the ablation catheter and the major coronary vessels; B: Superior left lateral view of the CARTO 3 activation map showing the LV summit and the LCC where ablation was delivered (red disc); C: Computed tomographic image of the LV summit (reproduced with permission from Lin et al.5). ABL, ablation; AIV, anterior interventricular vein; GCV, great cardiac vein; LAD, left anterior descending coronary artery; LCC, left coronary cusp; LCx, left circumflex coronary artery; LV, left ventricular; MAP, mapping; RCC, right coronary cusp; SP, septal perforator.
Given that the LV summit is situated proximal to several structures (LCC, right coronary cusp, the septal right ventricular outflow tract, aortic-mitral continuity, GCV/AIV junction), successful catheter ablation can be achieved from any of these structures (Figure 2C).1–3,5 Yamada et al.1 reported successful ablation of LV summit VA within the GCV/AIV in 14 of 25 patients with earlier local ventricular activation in the GCV/AIV than in any other endocardial site. However, and as in our patient, ablation through the coronary venous system may not be possible due to difficulty in advancing the ablation catheter to the site of interest, the proximity of coronary arteries or the inability to achieve adequate power. Jauregui Abularach et al.2 reported successful ablation from the LCC in 9 of 16 patients who had VA that were mapped marginally closer to GCV/AIV, describing an aVL/aVR Q-wave ratio < 1.45 to be predictive of successful ablation from the LCC (aVL/aVR Q-wave ratio was 1.33 in our patient). Finally, when ablation from the endocardium or the coronary venous system fails, a percutaneous epicardial approach may be considered. In a study of 23 such patients, epicardial ablation was attempted in 14 patients, being successful in only 5 of them, and in the remaining 9 patients, the VA origin was in the inaccessible area in close proximity to the major coronary vessels.3
In summary, we present a patient with PVC from the LV summit with best activation and pace maps at the GCV/AIV junction. However, due to anatomical restrictions, ablation was carried out successfully from the LCC.
CONFLICTS OF INTERESTM.A. Arias is an Associate Editor of Revista Española de Cardiología.