The aims of this study are to describe the mean values of carotid intima-media thickness and how it increases with age, and to compare carotid injury in diabetics and hypertensive patients with that of controls. We included 562 subjects (121 diabetics, 352 hypertensive patients, 89 controls). The mean intima-media thickness was 0.781mm in diabetics, 0.738mm in hypertensive patients and 0.686mm in controls. The difference in intima-media thickness between diabetics and controls and between hypertensive patients and controls, adjusted for age, was 0.040 and 0.026mm, respectively. We observed an increase in intima-media thickness of 0.005 mm in diabetics and of 0.005 mm in controls with every additional year of age. We found carotid damage in 23% of the diabetics, 12% of the hypertensive patients and 3.4% of the controls. In conclusion, the intima-media thickness is greater in diabetics, but the annual increase in the thickness is greater in hypertensive patients.
Keywords
Carotid intima-media thickness (IMT) is related to cardiovascular risk factors and diseases, and its measurement by means of ultrasound makes it possible to detect thickening in the initial phases of atherosclerosis.1, 2 For every 0.1-mm increase in carotid IMT, the relative risk of ischemic heart disease increases by 15% and that of cerebrovascular disease by 18%.3 In type 2 diabetes mellitus (DM2) patients, the carotid IMT is 0.13mm greater than in the controls. This implies an increase in age of 10 years, a circumstance that is related to a 40% higher cardiovascular risk.4 Hypertensive patients, even those in a state of prehypertension, have a greater carotid IMT than controls.5 In Spain, carotid IMT values in patients with no cardiovascular risk factors are available,6, 7 but we have no data on the carotid IMT in DM2 and hypertensive patients. The objective of this study is to compare the mean carotid IMT values and incidence of carotid injury in DM2 and hypertensive patients versus controls and to analyze the increase in carotid IMT with age.
MethodsWe performed a descriptive, cross-sectional study from December 2006 to June 2009. We included consecutively all patients between the ages of 25 and 80 years without previous cardiovascular disease referred to the research unit. The sample was comprised of 352 hypertensive patients, 121 diabetics and 89 individuals who had neither of these diseases. The protocol was approved by the Clinical Research Ethics Committee of the University of Salamanca and all the participants signed an informed consent form.
The clinical, anthropometric and analytical data collected are shown in Table 1. The measurement procedure has been described previously.8
Table 1. Clinical Characteristics, Traditional Risk Factors, Emerging Risk Factors and Carotid Intima-Media Values of the Groups of Subjects Included in the Study.
| Diabetics | Hypertensive patients | Controls | Diabetics versus controls, P | |
| Subjects, n (%) | 121 (21.5) | 352 (62.6) | 89 (15.8) | <.001 |
| Age, mean (SD), years | 60.23 (10.085) | 55.051 (1.333) | 50.531 (2.261) | <.001 |
| Sex | .168 | |||
| Men, n (%) | 79 (65.3) | 218 (61.9) | 47 (52.8) | |
| Women, n (%) | 32 (34.7) | 134 (38.1) | 42 (47.2) | |
| Traditional risk factors | ||||
| Smokers, n (%) | 30 (24.8) | 79 (22.4) | 27 (30.3) | .295 |
| Office SBP, mean (SD), mmHg | 136.22 (16.99) | 142.65 (16.92) | 125.20 (9.66) | <.001 |
| Office DBP, mean (SD), mmHg | 83.58 (9.77) | 90.91 (10.43) | 80.41 (6.44) | <.001 |
| Pulse pressure, mean (SD), mmHg | 53.09 (13.86) | 51.96 (13.39) | 44.95 (9.87) | <.001 |
| Heart rate, mean (SD), bpm | 73.46 (12.75) | 73.01 (12.33) | 73.19 (14.75) | .967 |
| BMI, mean (SD) | 29.77 (5) | 28.25 (3.64) | 26.79 (3.51) | <.001 |
| LDL-C, mean (SD), mg/dL | 112.96 (27.43) | 134.48 (33.69) | 131.70 (31.69) | <.001 |
| HDL-C, mean (SD), mg/dL | 50.60 (12.66) | 53.05 (13.03) | 55.39 (14.27) | .033 |
| Triglycerides, mean (SD), mg/dL | 135.90 (75.28) | 132.87 (80.23) | 114.57 (61.09) | .092 |
| Altered baseline blood glucose, mean (SD), mg/dL | 0.25 (0.43) | 0.14 (0.35) | 0.05 (0.23) | <.001 |
| Emerging risk factors | ||||
| Waist circumference, mean (SD), cm | 101.33 (12.68) | 97.58 (10.7) | 92.84 (11.26) | <.001 |
| Insulin resistance, mean (SD), μU/mL (HOMA index) | 4.07 (4.07) | 2.43 (1.94) | 2.01 (1.56) | <.001 |
| C-reactive protein, mean (SD), mg/dL | 0.27 (0.41) | 0.27 (0.4) | 0.18 (0.18) | .199 |
| Plasma fibrinogen, mean (SD), mg/dL | 325.62 (60.12) | 316.10 (63.33) | 307.63 (71.1) | .156 |
| Common carotid artery ultrasound | ||||
| Maximum mean carotid IMT, mean (SD), mm | 0.985 (0.27) | 0.940 (0.17) | 0.816 (0.12) | <.001 |
| Minimum mean carotid IMT, mean (SD), mm | 0.628 (0.09) | 0.590 (80.08) | 0.568 (0.08) | <.001 |
| Average maximum carotid IMT, mean (SD), mm | 0.964 (0.14) | 0.910 (0.12) | 0.850 (0.1) | <.001 |
| Highest maximum carotid IMT, mean (SD), mm | 1.237 (0.3) | 1.161 (0.2) | 1.065 (0.15) | <.001 |
| Lowest maximum carotid IMT, mean (SD), mm | 0.749 (0.11) | 0.713 (0.1) | 0.670 (0.1) | <.001 |
| Average mean carotid IMT, mean (SD), mm | 0.781 (0.11) | 0.737 (0.1) | 0.686 (0.09) | <.001 |
| Carotid injury, * n (%) | 28 (23.1) | 43 (12.2) | 3 (3.4) | <.001 |
BMI, body mass index; DBP, diastolic blood pressure; HDL-C, high-density lipoprotein cholesterol; HOMA, Homeostasis Model Assessment; IMT, intima-media thickness; LDL-C, low-density lipoprotein cholesterol; SBP, systolic blood pressure; SD, standard deviation.
* Carotid injury: if the mean carotid IMT was >0.9mm and/or there were arteriosclerotic plaques (carotid IMT≥1.5mm).
Two trained researchers measured the carotid IMT, and reliability was evaluated prior to beginning the study by means of the intraclass correlation coefficient, with values of 0.974 for intraobserver agreement with regard to repeated measurements in 20 subjects, and 0.897 for interobserver agreement. To optimize reproducibility, we employed a SonoSite Micromaxx ultrasound system (SonoSite Inc, Bothell, Washington, United States) using a 5-10MHz multifrequency high-resolution linear transducer with the Sonocal software package to perform automated measurements of the mean and maximum carotid IMT, with a discrimination limit expressed in microns. The measurements were carried out in common carotid artery, with the subject lying down, neck extended and head slightly turned in the direction opposite to the carotid artery being examined. A 10-mm longitudinal section located at a distance of 1cm from the bifurcation was studied and measurements were performed in the proximal and distal walls in lateral, anterior and posterior projections, along an axis perpendicular to the artery, to establish two lines: the intima-media interface and the media-adventitia interface. A total of six measurements were obtained in each carotid artery, and the average mean and maximum values were recorded. We considered vascular injury to be present when the mean carotid IMT was greater than 0.9mm or arteriosclerotic plaques (carotid IMT greater than or equal to 1.5mm) were detected.9 The researchers who performed the ultrasound had no data on the patient.
Statistical AnalysisThe quantitative variables are expressed as measures of central tendency and dispersion and the categorical variables as percentages. We assessed the association between qualitative variables with the chi-square test and between-group differences in means using analysis of variance (ANOVA) and, as a post hoc test, that of Scheffe, with an alpha value of .05. We controlled for the effect of age in the comparison of the means by analysis of covariance (ANCOVA).
We determined the influence of age on carotid IMT using multivariate linear regression analysis, establishing four models: model 1, adjusting for age; model 2, adjusting for age and sex; model 3, adding the traditional risk factors (smoking habit, systolic blood pressure, diastolic blood pressure, pulse pressure, heart rate, body mass index, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, triglycerides and baseline blood glucose), and model 4, adding the emerging risk factors (waist circumference, C-reactive protein, plasma fibrinogen and insulin resistance evaluated using the HOMA [Homeostasis Model Assessment] index). We identified the variables associated with the presence of carotid injury by means of logistic regression analysis. In the equation, we included as independent variables those used in the multiple linear regression model. We employed the SPSS/PC+ 17.0 statistical software package.
ResultsThe traditional and emerging risk factors and the ultrasound variables are shown according to groups in Table 1. The difference in carotid IMT between diabetics and controls was 0.095mm (95% confidence interval [CI], 0.058-0.132); between hypertensive patients and controls, 0.052mm (95% CI, 0.020-0.084), and between diabetics and hypertensive patients, 0.043mm (95% CI, 0.012-0.071). Adjusting these differences for age by means of ANCOVA, we observed differences in the carotid IMT of 0.040mm between diabetics and controls and 0.026mm between hypertensive patients and controls (P<.05). However, between diabetic and hypertensive patients, the difference was 0.013mm (P>.05).
Multiple linear regression analysis showed that, in diabetics, for every one-year increase in age we can expect an increment in carotid IMT of 0.005mm in the first three models and of 0.004mm upon adding the emerging risk factors in model 4. In hypertensive patients, the increment in carotid IMT for every one-year increase in age remains constant in the four models (0.006mm). In the controls, the beta coefficient ranged from 0.004mm to 0.006mm, and the greatest increment in carotid IMT was produced when adjustment was made for sex (0.006mm); upon adjustment for the traditional and emerging risk factors, the increase in carotid IMT was 0.005mm and 0.004mm, respectively (Table 2).
Table 2. Multiple Regression Analysis of the Carotid Intima-Media Thickness in Diabetics, Hypertensive Patients and Controls According to Different Models.
| β (95% CI) | P | |
| Diabetics | ||
| Model 1: age | 0.005 (0.003-0.007) | <.001 |
| Model 2: age and sex | 0.005 (0.004-0.007) | <.001 |
| Model 3: age, sex and traditional risk factors | 0.005 (0.002-0.008) | <.001 |
| Model 4: age, sex, traditional risk factors and emerging risk factors | 0.004 (0.001-0.008) | .014 |
| Hypertensive patients | ||
| Model 1: age | 0.006 (0.005-0.007) | <.001 |
| Model 2: age and sex | 0.006 (0.005-0.007) | <.001 |
| Model 3: age, sex and traditional risk factors | 0.006 (0.005-0.007) | <.001 |
| Model 4: age, sex, traditional risk factors and emerging risk factors | 0.006 (0.005-0.007) | <.001 |
| Controls | ||
| Model 1: age | 0.005 (0.004-0.007) | <.001 |
| Model 2: age and sex | 0.006 (0.004-0.007) | <.001 |
| Model 3: age, sex and traditional risk factors | 0.005 (0.002-0.008) | <.001 |
| Model 4: age, sex, traditional risk factors and emerging risk factors | 0.004 (0.003-0.008) | <.001 |
CI: confidence interval.
Dependent variable: average mean carotid intima-media thickness. Reference variable: age. Model 1: adjusted for age. Model 2: adjusted for age and sex. Model 3: adjusted for age, sex and traditional risk factors (smoking habit, office systolic blood pressure, office diastolic blood pressure, pulse pressure, heart rate, body mass index, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, triglycerides and altered baseline blood glucose). Model 4: adjusted for age, sex, traditional risk factors and emerging risk factors (waist circumference, C-reactive protein, plasma fibrinogen and HOMA [Homeostasis Model Assessment] index).
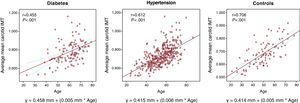
According to the linear regression line (Figure 1), the carotid IMT increased by 0.005mm for every year of age in diabetics and in controls, and by 0.006mm per year in hypertensive patients, but diabetic and hypertensive patients had higher carotid IMT values at the start of the study.
Figure 1. Simple linear regression lines, regression equations and r and P values showing the correlations between mean intima-media thickness and age in diabetics, hypertensive patients and controls.
In the logistic regression analysis, using the presence of carotid injury as a dependent variable and age as a reference variable, in diabetics, for each one-year increase in age, the odds ratio (OR) for presence of carotid injury was 1.05 (95% CI, 1-1.11; ß=0.052; P=.041) in model 1 and 1.06 (95% CI, 1-1.11; ß=0.057; P=.032) in model 2, with no significant changes in models 3 and 4. In hypertensive patients, in model 1, the OR was 1.12 (95% CI, 1.07-1.16; ß=0.112; P<.001); in model 2, OR=1.12 (95% CI, 1.08-1.17; ß=0.115; P<.001); in model 3, OR=1.22 (95% CI, 1.06-1.61; ß=0.276; P=.002); and in model 4, OR=1.39 (95% CI, 1.06-1.61; ß=0.276; P=.007); the controls were not included because only three subjects had carotid injury.
DiscussionOur study shows that the carotid IMT and the incidence of carotid injury are greater in diabetics; hypertensive patients have intermediate values and the controls, lower; the differences in carotid IMT are maintained after adjustment for age.
Patients with DM2 have an average mean age-adjusted carotid IMT 0.04mm greater than the controls, a value lower than that reported by Brohall et al,4 who measured the carotid IMT in predefined segments (0.09mm). The difference between hypertensive patients and controls in terms of carotid IMT is 0.026mm, with an annual increment of 0.006mm. These findings are similar to those of Puato et al5 with respect to the difference in carotid IMT, but lower than the annual mean increment of 0.11mm over 5 years of follow-up.
The data in Spain in individuals without risk factors6, 7 reflect an increase in the annual mean carotid IMT of 0.005mm and 0.006mm per year, similar to the controls in this report. In the United States,3 based on annual carotid IMT measurements, a yearly progression of 0.010mm has been estimated and, in Japan,10 this value is 0.006mm. The differences can be explained, in addition to the origin of the population, by the method utilized and the segment of carotid examined. One noteworthy observation is the loss of influence of age on carotid IMT upon adjustment for the traditional and emerging risk factors among diabetic subjects and controls, there being no clear explanation for this circumstance, although it is probably due to the fact that, from the time they receive the diagnosis of their disease, the majority of diabetic individuals are being treated with statins, drugs that reduce the carotid IMT; nevertheless, it is a finding that needs to be confirmed in prospective studies.
In conclusion, the carotid IMT is greater in diabetics, but the annual increase in thickness is higher in hypertensive patients.
FundingThis article is based on the study entitled “Lesión de órganos diana y monitorización ambulatoria de la presión arterial (LOD-RISK)”, and its different phases and subprojects have been financed by the regional healthcare administration (GRS/47-05, GRS/167/A/07 and GRS/254/A/08), by the Consejería de Sanidad de la Junta de Castilla y León, Spain, (SAN/196/SA36/07) and by ISCIII-RETICS, cofinanced with FEDER funds (RD06/0018).
Conflicts of interestNone declared.
Received 21 May 2010
Accepted 17 October 2010
Corresponding author: Unidad de Investigación, Centro de Salud La Alamedilla, Avda. Comuneros 27-31, 37003 Salamanca, Spain. magomez@usal.es