Relatively little is known on how the Doppler method compares with oscillometric measurement using a conventional automatic blood pressure device to determine the ankle-brachial index, when determinations are performed by physicians with little experience. To assess the diagnostic efficacy of both methods in this professional group, we calculated their sensitivity, specificity, and positive and negative predictive value in 158 legs of 85 patients with symptoms of intermittent claudication. Angiography was used as the gold standard. Of the legs examined, 131 showed significant arterial obstruction. The oscillometric method showed 97% sensitivity, 89% specificity, 98% positive predictive value, and 86% negative predictive value. The Doppler method showed 95% sensitivity, 56% specificity, 91% positive predictive value, and 68% negative predictive value. This study suggests that the automatic blood pressure equipment has greater diagnostic accuracy when the test is performed by physicians not specifically trained to use the Doppler probe.
Keywords
Given that it is asymptomatic in over 50% of cases, peripheral arterial disease (PAD) is underdiagnosed.1 The high cardiovascular morbidity and mortality associated with a diagnosis of PAD make early detection essential if therapies aimed at halting its progression are to be implemented.2 Currently, there are no evaluation methods available which provide a quick and accurate diagnosis of the disease, although determination of the ankle-brachial index (ABI) provides a highly reliable diagnosis.3 The usual way of calculating this index is to use a manual sphygmomanometer and a Doppler probe to assess blood flow. The ABI is the ratio obtained by dividing the highest systolic blood pressure in the ankle by the highest systolic blood pressure in the upper extremities. The main disadvantages of the method are that it requires a substantial amount of time, a Doppler device is specifically required, and prior training is required to avoid high inter-observer variability.4, 5 This leads to a lack of systematic measurement of ABI in primary care.
Several attempts have been made to simplify the test's implementation by replacing the ultrasonic probe of the classic Doppler method (DM) with automated commercial machines which use the oscillometric method (OM) to calculate systolic blood pressure quickly and objectively.6, 7, 8 In this study to determine the diagnostic accuracy of each technique, three medical residents determined ABI using the DM and OM after a short training period. The results were compared to those obtained using angiography.
MethodsA total of 85 patients over 30 years of age referred to the catheterization laboratory for angiography for peripheral arterial intermittent claudication or suspected advanced PAD were included consecutively in the study.
AIB MeasurementThe Doppler measurement was performed using an 8MHz Doppler probe Doplex II MD2/SD Huntleigh model and a sphygmomanometer with appropriate size cuffs. The oscillometer used was an Omron M4-I. The ABI was calculated as the ratio of peak systolic pressure at the ankle and arms. We excluded patients with non-compressible arteries with an ABI>1.4. If the OM still gave an error reading after three serial attempts with rehabilitation of cuff pressures, pressure was assumed to be <60 mmHg and a “0 index” was assigned. A “0 index” was also assigned if it was not possible to detect flow with the DM.
AngiographySequential images were performed using the digital subtraction technique. Severity was determined simultaneously by visual comparison between healthy and diseased segments and by using the Quantitative Coronary Angiography (QCA) program. Hemodynamically significant or severe PAD was defined as stenosis with ≥50% obstruction and non-significant PAD as <50% obstruction.
Statistical AnalysisThe data were analyzed using SPSS13.0 software (Chicago, Illinois, USA). Continuous variables were expressed as mean±standard deviation and categorical variables as percentages. To determine the reliability of the ABI in diagnosing PAD, we calculated the sensitivity, specificity, positive predictive value, negative predictive value, and the area under the ROC curve. The results of standard angiography were used as the gold standard.
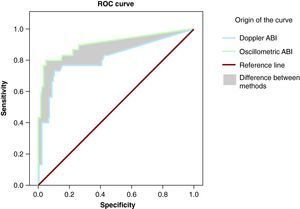
ResultsA total of 85 patients were included (Table 1, Table 2). Twelve legs were excluded, for a variety of reasons: 6 cases because of amputation, 4 due to painful ulcers which ruled out examination, and 2 because the ABI was >1.4. In total, 158 legs were analyzed. Based on our angiographic criteria, 131 legs (83%) were diagnosed with PAD. OM gave 3 false positives and DM 12, together with 4 and 7 false negatives, respectively. The area under the curve (AUC) for the OM, including the “0 index” (Figure 1), was 0.94 (95% confidence interval [CI], 0.85 to 1.03); sensitivity was 97% (93%-99%), specificity 89% (67%-95%), positive predictive value 97% (94%-99%), and negative predictive value 86% (63%-93%). For the DM, the AUC was 0.81 (95% CI, 0.67 to 0.94), while sensitivity was 95% (89%-97%), specificity 56% (33%-70%), positive predictive value 91% (85%-95%), and negative predictive value 68% (43%-82%).
Table 1. Demographic Characteristics.
| Patients | 85 |
| Age | 68±11 |
| Male | 76 (89) |
| High blood pressure | 65 (76) |
| Diabetes mellitus | 44 (52) |
| Hypercholesterolemia | 37 (43.5) |
| Current smokers | 27 (32) |
| Ex-smokers | 39 (46) |
| Ischemic heart disease | 24 (30) |
| Percutaneous coronary interventionism | 10 (12) |
| Coronary surgery | 5 (6) |
| Previous stroke | 18 (22) |
| Carotid revascularization | 2 (2.4) |
| Aortic aneurism | 5 (6) |
Data are expressed in n (%) or mean±standard deviation.
Table 2. Angiographic Characteristics.
| Legs | 158 |
| Non-significant stenosis (<50%) | 27 (17) |
| Significant lesion (≥50%) | 131 (83) |
| Isolated proximal lesion >50% | 14 (8.8) |
| Isolated medial lesion >50% | 12 (7.5) |
| Isolated distal lesion >50% | 11 (7) |
| Total proximal lesions >50% | 72 (45.5) |
| Total medial lesions >50% | 99 (62.6) |
| Total distal lesions >50% | 89 (56.3) |
Distal, tibiofibular; Medial, femoropopliteal; Proximal, aortoiliac.
Figure 1. Diagnostic performance of the ankle-brachial index using Doppler and oscillometric methods. ABI, ankle-brachial index.
DiscussionIn these patients, the diagnostic accuracy of OM was found to be superior to DM in determining the ABI when performed by doctors who had not received specific training in Doppler testing. However, as reported by other authors,6, 8 very severe angiographic lesions lead to very low blood pressure (<70 mmHg) which is not detectable using currently available, validated commercial automated devices.
The Omron device was unable to measure blood pressure in 70 legs after three serial attempts with cuff rehabilitation to a “0 index”. However, severe angiographic lesions were present in 69 of these 70 legs. The strong association between severe arterial lesions and the impossibility of calculating systolic blood pressure after several attempts with the OM suggests a new criterion to predict the severity of arterial obstruction.
Using the DM, we did not detect tibial or dorsalis pedis pulse in 55 legs with severe angiographic lesions. We were, however, able to distinguish values of <60 mmHg in 9% of the affected legs. This finding represents a clear advantage over the oscillometric method, as it means the device can detect very low blood pressures in the lower limbs. The main inconvenience of the DM is inter-observer variability; being able to locate the pulse with the Doppler is directly related to the expertise of the clinician carrying out the exploration.4, 5 In the present study, we were unable to capture a tibial or dorsalis pedis pulse using Doppler in 12 legs with normal vessels or non-significant lesions, from a total of 27. This lack of expertise in capturing a theoretically normal pulse is what led to a specificity of barely 56%.
When the “0 index” is included in the analysis, the results were better for OM (97% sensitivity; 89% specificity) than for the DM (95% sensitivity; 56% specificity).
The main limitations of the study are the low number of patients studied and the bias introduced by including patients with intermittent claudication or suspected advanced PAD. The high prevalence of PAD in the patients included directly influenced the predictive values obtained, so the results cannot be extrapolated to the general population. Larger studies in this type of population are needed to confirm these results, but we consider it questionable to perform angiographies in patients without PAD only to evaluate the efficacy of the method.
Previous studies in the general population3, 9, 10 showed variable results when using the DM as a reference to evaluate the security and efficacy of OM. Using DM as the reference technique limits the conclusions of those studies because interobserver variability cannot be avoided, even when the measurement is carried out by experts.
The strength of our study is that we used peripheral angiography as the standard in determining the presence of arterial lesions; that allowed us to confirm the relationship that exists between the “0 index” and the severity of the lesions, independently of the expertise of the investigating clinician or the method used.
The results indicate that automatic blood pressure measuring equipment has better diagnostic accuracy when doctors not specially trained in the use of the Doppler probe carry out the testing.
Conflicts of interestNone declared.
Received 4 May 2010
Accepted 14 October 2010
Corresponding author: Londres 30, 4.o B, 10005 Cáceres, Spain. jorgevegafernandez@gmail.com