Determination of cardiac sympathetic innervation status, using 123I-metaiodobenzylguanidina (123I-MIBG) scintigraphy, could improve risk stratification for ventricular arrhythmias in patients with heart failure and reduced left ventricular ejection fraction (LVEF).1 Myocardial washout (WO) reflects the degree of sympathetic activity: a high value reflects hyperactivity and excess noradrenaline release.2 The late (4 hour) heart-to-mediastinum (H/M) ratio reflects the status of the synaptic terminals: a low value indicates sympathetic denervation and reduced noradrenaline reuptake.2
We studied 36 patients with symptomatic heart failure (New York Heart Association functional class II), LVEF < 35% and optimized treatment, who had an implantable cardioverter-defibrillator (ICD) in primary prevention (median = 4.7 [interquartile range, 2.0-5.9] years since implantation): 18 patients had at least 1 appropriate therapy and 18 had no therapies. To avoid bias, we excluded patients with decompensated heart failure, infarction, or coronary revascularization in the past year, those aged < 18 or > 70 years, with severe pulmonary disease, creatinine > 2mg/dL, diabetes mellitus with organ damage, or on treatment with alpha-blockers. The study was approved by the local Ethics Committee, and written informed consent was obtained. Patients received an intravenous injection of 10 mCi (370 MBq) of 23I-MIBG (AdreView, GE Healthcare) and planar images were acquired of the anterior thorax at 15minutes and at 4hours. Quantification of the early and late H/M ratio and WO was performed blinded. After scintigraphy (median, 4.2 [3.2-5.0] years), 1 patient from the no-therapy group died prematurely from sepsis and 2 received therapies, therefore the final sample was 15 with no therapy and 20 with therapy: 75% received shocks and 25% received antitachycardia pacing only. The final follow-up was a median of 9.1 [6.3-10.2] years after ICD implantation.
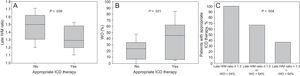
The values for early H/M ratio, late H/M ratio, and WO were 1.45 ± 0.17, 1.37 ± 0.18, and 32% ± 26%, respectively. The late H/M ratio was lower in patients with a previous infarct (1.32 ± 0.16 vs 1.5 ± 0.16; P = .005) and was correlated with LVEF (r = 0.4; P = .016); there were no other correlations between parameters and patient characteristics. When we compared patients with therapy vs patients without (Table 1), the late H/M ratio was lower (1.32 ± 0.17 vs 1.45 ± 0.18; P = .039) and the WO was higher (40.2 ± 29 vs 21.2 ± 16.6; P = .021) in the group with therapy (Figure 1), while the early H/M ratio was similar (1.43 ± 0.15 vs 1.47 ± 0.20; P = .5). When we looked only at shock therapy, the late H/M ratio lost significance (1.31 ± 0.14 vs 1.43 ± 0.20; P = .068) and the WO increased (45 ± 29 vs 17 ± 21; P = .007). ROC curve analysis showed an area under the curve of 0.70 (95% confidence interval [95%CI], 0.52-0.84; P = .021) for late H/M ratio and 0.68 (95%CI, 0.5-0.83; P = .043) for WO. The optimal cutoff point was ≤ 1.3 for late H/M ratio (55% sensitivity, 80% specificity) and > 54% for WO (45% sensitivity, 100% specificity). On analysis of the combined variable (late H/M ratio ≤ 1.3 and/or WO > 54%), 100% of patients with abnormalities in both parameters received therapy (n = 7), as did 67% of those with just 1 abnormality (n = 9), and 37% (n = 19) of those with no abnormalities (P = .004) (Figure 1). After scintigraphy (n = 12), these rates were 100%, 44%, and 10%, respectively (P = .007). The ordinal combined variable maintained significance after adjusting for LVEF, infarction, age, N-terminal pro-brain natriuretic peptide, QRS, and end-diastolic volume (OR = 12.55; 95%CI, 1.51-104.26; P = .019).
Characteristics of Patients With and Without Appropriate ICD Therapy
| Appropriate therapy | P | ||
|---|---|---|---|
| Yes (n = 20) | No (n = 15) | ||
| Age, y | 64 ± 9 | 64 ± 8 | .803 |
| Male | 19 (95) | 14 (93%) | .839 |
| Weight, kg | 91 ± 14 | 91 ± 24 | .989 |
| Height, cm | 171 ± 11 | 164 ± 24 | .274 |
| Systolic blood pressure, mmHg | 118 ± 15 | 123 ± 17 | .367 |
| Diastolic blood pressure, mmHg | 66 ± 7.4 | 68 ± 8 | .774 |
| Heart rate, bpm | 68 ± 11.2 | 67 ± 8 | .753 |
| Atrial fibrillation | 3 (15) | 2 (13%) | .153 |
| QRS, ms | 158 ± 31 | 131 ± 29 | .018 |
| Previous infarct | 13 (65) | 11 (73%) | .612 |
| Diabetes mellitus | 10 (50) | 8 (53%) | .692 |
| Renal failure | 10 (50) | 6 (40%) | .570 |
| Cardiac resynchronization therapy | 9 (45) | 6 (40%) | .775 |
| Left ventricular ejection fraction, % | 29 ± 6 | 31 ± 9 | .544 |
| End-diastolic left ventricular volume, mL | 224 ± 97 | 166 ± 76 | .043 |
| Left atrial volume, mL/m2 | 48 ± 19 | 41 ± 21 | .322 |
| Creatinine, mg/dL | 1.27 ± 0.33 | 1.21 ± 0.32 | .610 |
| Urea, mg/dL | 57.2 ± 21 | 54.4 ± 15.5 | .680 |
| Calcium, mg/dL | 9.3 ± 0.46 | 9.5 ± 0.5 | .175 |
| Total bilirubin, mg/dL | 0.74 ± 0.42 | 0.72 ± 0.37 | .918 |
| Total cholesterol, mg/dL | 155 ± 26 | 155.9 ± 47.5 | .985 |
| GGT, U/L | 48 ± 53 | 54 ± 54 | .760 |
| Sodium, mEq/L | 138 ± 3 | 140 ± 3 | .146 |
| NT-proBNP, pg/mL | 789 [629-1553] | 665 [315-1239] | .020 |
| Troponin T, pg/mL | 10 (5-19) | 16 (10-23) | .752 |
| Magnesium, mg/dL | 2.0 ± 0.25 | 2.0 ± 0.39 | .332 |
| Thyrotropin, μIU/mL | 1.7 ± 0.8 | 1.9 ± 0.84 | .590 |
| Hemoglobin, g/dL | 14 ± 1.8 | 14 ± 1.1 | .711 |
| ACEI/ARB-II | 20 (100) | 15 (100) | 1 |
| Beta-blockers | 30 (100) | 15 (100) | 1 |
| Digoxin | 4 (20) | 3 (20) | 1 |
| Diuretics | 20 (100) | 15 (100) | 1 |
| Aldosterone blockers | 16 (80) | 13 (87) | .600 |
ACEI, angiotensin-converting enzyme inhibitor; ARB-II, angiotensin II receptor blocker; GGT, gamma glutamyl transferase; NT-proBNP: N-terminal pro-brain natriuretic peptide.
Data are expressed as No. (%), mean ± standard deviation, or median [interquartile range].
In a meta-analysis of 18 studies (1755 patients), a low late H/M ratio or a high WO were shown to be independently associated with increased risk of adverse cardiac events.3 The AdreView Myocardial Imaging for Risk Evaluation in Heart Failure (ADMIRE-HF) study (symptomatic heart failure with LVEF < 35%) found that a late H/M ratio < 1.2 was associated with ventricular arrhythmias.1 In patients with an ICD, a lower late H/M ratio was associated with appropriate therapy,4 as was higher WO in a study of 25 patients.5 In comparison with previous studies, ours had a longer follow-up (median 9.1 years after ICD implantation), whereas in others follow-up has been < 3 years.1,4,5 In addition, this study included patients with ICD in primary prevention, and only the study by Boogers et al.4 included a majority (103 or 116) with ICD in primary prevention. Our study also shows that both parameters, late H/M ratio and WO, provide complementary information and that their combination could be the best approximation to identify the probability of receiving therapy (100% of patients with abnormalities of both variables received therapy, even after scintigraphy), a point not identified in other studies.
Our study has some limitations, for example, the findings cannot be extrapolated to the time of implantation, given that scintigraphy was done later and at a variable time. The small sample means that the findings must be interpreted in the context of other studies, in particular the ADMIRE-ICD trial (NCT02656329), which will assess the value of the late H/M ratio in the indication for ICD in primary prevention with LVEF 30-35%.
FUNDINGFunds from the Instituto de Salud Carlos III (RD12/0042/0049; Red de Investigación Cardiovascular en Insuficiencia Cardiaca [Heart Failure Cardiovascular Research Network]) (INT 15/00108, 16/00172), and an unconditional grant from GE Healthcare.
CONFLICTS OF INTERESTD.A. Pascual-Figal has received a research grant from GE Healthcare.