Keywords
INTRODUCTION
Coronary artery perforation is a rare complication of coronary surgery that generally occurs when the guidewire crosses complex lesions or when devices such as an atherotome or laser are used.1,2 The more frequent use of platelet glycoprotein IIb/IIIa receptor inhibitors (GPIIb/IIIa) greatly increases the risk of severe hemorrhaging, which can cause acute cardiac tamponade which is of difficult management. We report on a patient treated with abciximab who presented perforation of a distal branch of the right coronary artery during angioplasty, followed by acute cardiac tamponade. Pericardial bleeding was resolved by placement of 2 metal coils in the distal lumen of the vessel.
CASE STUDY
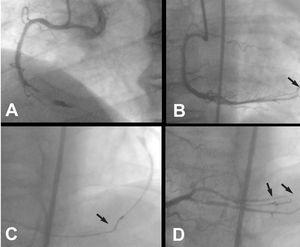
A 50-year-old man with a history of smoking and exertional angina of one week evolution presented in the emergency department at night for precordial pain at rest. The electrocardiogram (ECG) showed ascending ST segment elevation of 1 mm, with the J point on the isoelectric line, and Q wave in leads II and III. Creatine kinase elevation was 471 U/L. The patient was diagnosed with acute inferior wall myocardial infarction, and transferred, asymptomatic, to the coronary care unit. Coronary angiography was performed 12 hours after admission; thrombotic obstruction of the middle right coronary artery (RCA) was visualized, indicating the need for angioplasty. Sodium heparin (7000 U) was administered intravenously along with abciximab in a bolus dose of 0.25 mg/kg weight, followed by continuous perfusion at 10 μg/min. After crossing the occlusion with a hydrophilic-coated guidewire 3 aspirations using a 1.5 mm diameter X-Sizer thrombectomy device was performed (Figure 1A). Two coronary stents of 2.75x14 mm in the distal third and 3.0x18 mm in the middle third were subsequently implanted with good results. However, one of the immediate coronary angiographies showed thread-like extravasation of contrast material at the distal end of a distal arteriole of the right coronary artery (Figure 1B). Shortly afterwards, the patient presented sudden hypotension (40 mm Hg) due to cardiac tamponade that required emergent pericardiocentesis and drainage, which yielded 600 mL of blood. Protamine was administered and abciximab perfusion was discontinued. Mechanical hemostasis was accomplished by inflating a 1.5 mm diameter angioplasty balloon in the branch of the posterolateral artery proximal to the perforation. Multiple inflations were performed at low atmospheres for 4-5 min. Since extravasation of contrast medium to the pericardium persisted, a metal coil (Vortx® Fibered Platinum, Boston Scientific, Natick, Massachusetts, USA) was placed using a 2.3 Fr catheter (Rapid Transit, Cordis, Miami, Florida, USA) located in the distal branch of the perforated right coronary artery (Figure 1C). Because a small thread-like extravasation still persisted, a second coil was implanted. The absence of extravasation was confirmed in a repeat angiography (Figure 1). The ECG showed persistence of Q-wave in leads II and III, as well as a slight ST segment alteration in the posterolateral inferior wall, with posterior and lateral normalization after transfusion of packed red blood cells. Troponin values were positive. The following morning, the echocardiogram showed no pericardial effusion, and the drainage was removed. The patient was discharged at 48 hours. Four months later, stress testing was negative for ischemia.
Fig. 1. A: right coronary artery after thrombectomy. An image suggestive of intracoronary thrombus is observed. B: thread-like extravasation of contrast material to the pericardium (arrow) due to perforation of a distal arteriole by the angioplasty guidewire. C: fluoroscopic image showing placement of a metal coil (arrow) in the perforated vessel. D: resolution of extravasation image after placement of a second coil (arrows).
DISCUSSION
The incidence of cardiac perforation during angioplasty is 0.2%, but can be as high as 3% when devices such as an atherotome or laser are used.1,3 In 20% of cases,1 the angioplasty guidewire is the cause. According to Ellis et al,4 cardiac perforation can be classified into one of four types: Type I: extraluminal crater without extravasation; Type II: pericardial or myocardial blushing without contrast streaming; Type III: extravasation through perforation >1 mm with contrast streaming, and Type CS: cavity spilling when the extravasation streams toward an anatomical cavity. Although perforation may not result in symptoms and may be contained, it sometimes causes serious acute complications such as cardiac tamponade, myocardial infarction, malignant arrhythmias, and occasionally death. Early onset of pericardial effusion is associated with a worse prognosis since one third of these patients require emergent surgery, either because pericardiocentesis is ineffective or because the arterial injury must be repaired.1,5
Coronary artery perforation is more frequent when hydrophilic-coated guidewires are used, as occurred with our patient. These guidewires are very useful for crossing severe stenoses, but are unfortunately associated with a higher risk of arterial perforation, particularly when trying to cross complex lesions such as occlusions, bifurcations, long lesions, and tortuous vessels.6 In the patient we describe, the mechanism causing the perforation could have been the hydrophilic-coated guidewire or the inadvertent advance of the guidewire during the thrombectomy. On occasions, protamine administration and prolonged balloon inflation are enough to stop the bleeding.1,2 However, treatment with GPIIb/IIIa inhibitors limits the effectiveness of these hemostasis mechanisms. In patients in whom the extravasation is located in the wall of a small or large epicardial artery, it is usually effective to cover the perforation with a stent-graft.7 Nevertheless, in tertiary branches, arterioles or small distal vessels, other therapeutic measures aimed at occlusion of the distal vessel by either thrombosis or embolization are necessary. In addition to coils,8 precoagulated autologous blood, gelfoam and intracoronary thrombin have been used for this purpose in isolated cases.9-11 In our patient we used 2 platinum coils to stop the bleeding to the pericardium. The small changes in enzyme levels we observed after placing the coils were attributed to implantation as distal as possible in the posterolateral artery branch, thereby compromising a small amount of myocardial tissue, as well as the possibility that some infarcted tissue was already present in part of the territory. We should point out that the use of these devices, which are prone to thrombosis, should be limited to perforations of distal arterioles because they produce complete occlusion of the vessel lumen, with the resulting risk of infarction. This technique has recently been used as a successful elective procedure to occlude the first septal branch of the left anterior descending artery, in order to cause septal infarction in patients with hypertrophic obstructive cardiomyopathy.12
In summary, the technique we describe has the advantage of being fast and effective in sealing coronary perforation of a distal arteriole, avoiding the need for emergent surgery.
Correspondence: Dr. V. Martí.
Unidad de Hemodinámica. Servicio de Cardiología.
Hospital de la Santa Creu i Sant Pau.
Avda. Antoni M. Claret, 167. 08025 Barcelona. España.
E-mail: 18461vmc@comb.es