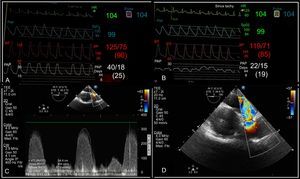
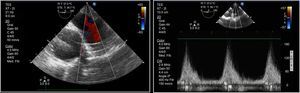
We report the case of a 41-year-old man, who was an active smoker, with no prior history of cardiac conditions or other history of interest, and who was admitted to hospital for anterior ST-elevation myocardial infarction in Killip class IV. During admission, he experienced cardiac arrest unresponsive to advanced cardiopulmonary resuscitation. Peripheral venoarterial extracorporeal membrane oxygenation was used initially during the arrest and was subsequently switched to central extracorporeal membrane oxygenation. Intra-aortic balloon counterpulsation was also required. Coronary artery disease was detected in 3 vessels with chronic occlusion of the circumflex artery and right coronary artery and acute occlusion of the proximal left anterior descending artery, which was revascularized with conventional stenting. After a favorable assessment and confirmation of the absence of serious neurological damage, the patient was placed on the heart transplant waiting list with top priority. Orthotropic heart transplant was finally performed with the Shumway technique (male 25-year-old donor weighing 80kg and 176cm tall for a recipient weighing 80kg and 178cm tall). After surgery, mild right ventricular dysfunction was observed (on rapid discontinuation of extracorporeal circulation), with progressive hemodynamic worsening at 24hours and a growing need for inotropic and vasopressor support. At 36hours, his liver enzymes were significantly elevated, and transesophageal echocardiography showed progression to severe dysfunction and dilatation of the right ventricle. Elevation of pulmonary pressures (measured with Swan-Ganz catheter before the anastomosis of the pulmonary artery and decline in the cardiac index to 1.9 L/min/m2) were observed with stenosis of the pulmonary artery anastomosis with a flow rate of > 3 m/s and maximum gradient of 38mmHg. In addition, severe tricuspid valve failure and extensive dilatation of the inferior vena cava with systolic flow reversal in the suprahepatic veins were also observed (Figure 1). Immediate surgery was performed (the chest was open due to hemorrhage after the intervention) to reconstruct the pulmonary artery anastomosis. Transesophageal echocardiography showed an immediate decrease in velocity across the anastomosis to 1.6 m/s and a notable improvement in right ventricular dysfunction (Figure 2). Vasoactive support could therefore be withdrawn and the patient was extubated.
A and B, Swan-Ganz catheter measurements. A: pulmonary hypertension according to pulmonary artery pressure prior to stenosis of the pulmonary artery anastomosis. B: normal pulmonary artery pressures after the stenosis of the pulmonary artery anastomosis. C: stenosis of the pulmonary artery anastomosis: flow > 3 m/s, maximum gradient 38mmHg. D: stenosis of the pulmonary artery along the short axis of the aortic arch at the level of the esophagus.
The main surgical technique in heart transplant is the Shumway-Lower technique,1 with end-to-end suture of the great vessels of the recipient and donor organs. It is important that the size mismatch between the donor organ and the recipient is not too large.2 Acute right ventricular failure accounts for 50% of postoperative cardiac complications and 20% of early mortality after heart transplant.3 Although the main causes of right heart failure are pressure or volume overload, myocardial ischemia, or arrhythmias, there have been 2 reports of stenosis of the pulmonary artery suture,4 an uncommon but reversible cause of right heart failure that occurs more frequently in the lung transplantation setting than the heart transplantation setting.5 In this complication, an etiological diagnosis and early treatment are essential to guarantee resolution. The complication is caused by mismatches in the size of the anastomosed vessels, suture constriction, intimal hyperplasia, or a combination of these. The consequences depend on the extent and site of the stenosis and the size of the affected vessel.4–6 Initial diagnosis can be made by echocardiography, preferably transesophageal; the great vessel view and the section of the aortic arch at the level of the upper esophagus provide the highest diagnostic yield and best quantification.3 One case has been reported with a satisfactory outcome after percutaneous treatment,4 as well as after surgery with anastomotic reconstruction. The second option was preferred in our patient because less than 36hours had elapsed since the first intervention and the chest was still open, thus facilitating rapid access to the anastomosis.
This case represents an uncommon complication that is not widely reported in the literature but which should nevertheless be considered in the differential diagnosis of acute right ventricular failure in heart transplantation.3 Likewise, it also reflects the importance of early diagnosis and treatment to avoid irreversibility. Anastomosis of the pulmonary artery should be assessed after withdrawal of extracorporeal circulation with transesophageal echocardiography, with the preferred views being the great vessel view and the aortic arch section at the level of the upper esophagus. Measurement of the gradient at the anastomosis with a Swan-Ganz catheter may also be useful.