Keywords
The present work examined the echocardiographic abnormalities of a sample of elderly patients, analyzing the differences between normotensive subjects, those with white coat hypertension (WCH), and those with sustained high blood pressure. The prevalence of WCH increases with age. It is estimated that some 43%-45% of people >65 years of age suffer this syndrome.1-4 The prevalence of left ventricular hypertrophy (LVH) in patients of this age approaches 15%.1-3 The presence of abnormalities in the shape of the left ventricle is associated with an increase in mortality.5-8 Despite the studies performed on WCH, its prognostic significance has remained unknown. The present work provides data on the repercussion of WCH in the elderly.
METHODS
The data examined in this work were gathered from a randomly selected subgroup of patients enrolled in the EPICARDIAN (EPIdemiología CARDIovascular en los ANcianos en España [Cardiovascular Epidemiology in Elderly Spanish People]) study. The methodology of the EPICARDIAN study has been described eslewhere.9 The baseline characteristics of the subgroup members were not significantly different from those of the original sample. Casual blood pressure (CBP) was determined in a physician's office using a mercury sphygmomanometer. Three measurements were taken using the same arm, 2 with the patient sitting and 1 with the patient standing. Ambulatory monitoring (24 h) was undertaken using a Spacelabs 90207 oscillometer. Normal blood pressure was regarded as a CBP of <140/90 mm Hg, no anti-hypertension treatment, and an ambulatory monitoring blood pressure of <135/85 mm Hg during activity. White coat hypertension was regarded as a systolic blood pressure (SBP) of ≥140 mm Hg and/or a diastolic blood pressure (DBP) of ≥90 mm Hg, no anti-hypertension treatment, and an ambulatory monitoring blood pressure of <135/85 mm Hg during activity. Sustained hypertension was regarded as an SBP of ≥140 and/or DBP ≥90 mm Hg, with hypertension treatment, and an ambulatory monitoring blood pressure of ≥135/85 mm Hg during activity. All echocardiograms were obtained using a Toshiba 160 apparatus equipped with a transthoracic transducer (2.5 MHz). The echocardiographers were unaware of the blood pressure conditions of the patients; the degree of agreement between them was determined. All echocardiographic measurements followed the norms of the American Society of Echocardiography published by Sahn et al10 in Circulation in 1978, and were performed in M and echo-Doppler modes. Left ventricular hypertrophy was deemed present when, if using the criteria of Deveraux,10 the ventricular mass index VMI (mass of the left ventricle/body surface area) was ≥134 g/m2 in men or ≥110 g/m2 in women, or if using the Framingham criteria10 the VMI (mass of the left ventricle/height) was ≥141 g/ m2 in men or ≥102 g/m2 in women, or if using the Cornell-Penn criteria10 the VMI (mass of the left ventricle/body surface area) was ≥111 g/m2 in men or ≥106 g/m2 in women. The prevalence of diabetes mellitus and dyslipidemia was not determined, nor was any treatment recorded that might have been prescribed for these conditions. Basic examinations were not performed.
Categorical variables were recorded as frequency distributions; continuous variables were recorded as means and their standard deviations. The χ2 or Fisher exact test was used to seek relationships between qualitative variables. ANOVA was used to compare the left ventricular mass (LVM) and VMI between groups. All calculations were performed using SPSS v.10 software.
RESULTS
Of 271 patients, 61 (22.5%) were classified as normotensive, 81 (29.9%) had WCH, and 129 (49.6%) had sustained high blood pressure. Table 1 shows the patients' demographic characteristics. The age distribution of the sample was: 172 subjects (63.5%) <75 years of age, and 99 (36.5%) ≥75 years of age. The left ventricular ejection fraction was 66.9% in the normotensive subjects, 67.7% in those with WCH, and 69.2% in those with sustained hypertension (P=.52). The LVM (g) was determined at 95% confidence interval (95% CI), and was 162 (95% CI, 136.1-187.9) in the normotensive subjects, 214.2 (95% CI, 198.1-231.4) in those with WCH, and 234.7 (95% CI, 214.9-254.4) in those with sustained hypertension (P=.0001). The VMI (g/m2) was 94.9 (95% CI, 82.3-107.6) in normotensive subjects, 125.6 (95% CI, 116.8-134.4) in those with WCH, and 136.3 (95% CI, 125.8-146.8) in those with sustained hypertension (P<.001). ANOVA detected significant differences between the three groups with respect to LVM (P<.001) and VMI (P<.001).
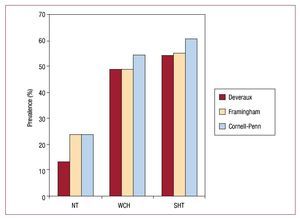
The prevalence of LVH (Figure 1) according to the Deveraux criteria was 13.2% in the normotensive patients, 49.1% in those with WCH, and 54.3% in those with sustained hypertension (P=.00007). According to the Framingham criteria this prevalence was 23.7% in the normotensive subjects, 49.1% in those with WCH, and 55.3% in those with sustained hypertension (P=.00012). According to the Cornell-Penn criteria, this prevalence was 23.7% in the normotensive subjects, 54.4% in those with WCH, and 60.6% in those with sustained hypertension (P=.00006).
Figure 1. General prevalence of left ventricular hypertrophy according to different criteria. NT: normotensive; SHT: sustained hypertension; WCH: white coat hypertension.
The sample was also examined according to age and sex. The prevalence of LVH was again determined according to the three sets of criteria outlined; Table 2 shows the results.
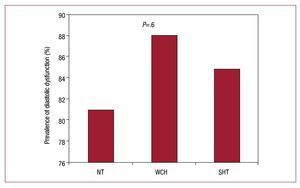
The prevalence of LVH was compared between normotensive patients and those with WCH, in general and according to age and sex. Significant differences (P<.005) were found in all cases except between women, when using the Framingham criteria (P=.2), and in subjects aged 75 and over when using the same criteria (P=.2). The same type of analysis was then performed to compare the prevalence of LVH in those with WCH and those with sustained hypertension. No significant differences were detected except between men when using the Framingham criteria (P=.03). Diastolic dysfunction was recorded in 81% of the normotensive patients, in 88.1% of those with WCH, and in 84.8% of those with sustained hypertension (P=.6) (Figure 2). The kappa index with respect to LVH was k=0.1.
Figure 2. Diastolic dysfunction in different subgroups. NT: normotensive; SHT: sustained hypertension; WCH: white coat hypertension.
DISCUSSION
Those studies that have examined morbidity/ mortality in patients with WCH have returned differing results.2,11 The best way to manage such patients is a matter of deabte.4,12 Despite the work undertaken to date, the prognostic significance of WCH has remained unknown.
The present work provides data on the repercussion of WCH in the elderly. The results suggest that WCH may be associated, in the long term, with cardiac damage between that associated with normotension and sustained hypertension; this potential relationship was maintained after stratifying by age and sex.
The prevalence of LVH in those patients with WCH was 49%. This is higher than that seen in the normotensive subjects but lower than that seen in those with sustained hypertension; this might have prognostic implications with respect to morbidity/ mortality.
The present results show that, in elderly people, WCH is associated with cardiac structural abnormalities more like those seen in patients with sustained hypertension than in normotensive subjects.
The kappa index for LVH showed a low level of agreement (κ=0.1). This is explained in that, when categorizing the quantitative variable VMI as the categorical variable LVH, much information is lost, a consequence of the large percentage of patients with a VMI slightly above the threshold for hypertrophy.
This study was funded by the FIS (93/0012-02, 96/1993-01, 970197 and 02/0896).
Correspondence: Dr. C. Suárez,
Servicio de Medicina Interna. Hospital Universitario de La Princesa. Diego de León, 62. 28006 Madrid. Spain
Received August 13, 2009.
Accepted for publication December 23, 2009.