Keywords
INTRODUCTION
Recent therapeutic advances have reduced mortality due to ischemic heart disease over the last 25 years1; this fact, in addition to an aging population, has increased the prevalence of chronic ischemic heart disease (CIHD).2
However, there is little available information on the clinical characteristics and prognosis of patients with CIHD in our area. This is especially true for identifying the prevalent clinical elements (such as diabetes mellitus [DM]) which are associated with a greater risk of complications during follow-up. These could help us come up with strategies to improve patient management.
The aim of the CIBAR Study is to describe demographic, clinical and therapeutic characteristics, and their impact on prognosis in a homogeneous cohort of outpatients with CIHD. We present said objectives in this subanalysis and assess the impact of DM.
METHOD
With the participation of 69 primary care physicians, during the month of February 2007 all patients that complied with the inclusion criteria were recruited into this prospective, multicenter cohort study. The exclusion criteria were: over 18 years of age, previous diagnosis of ischemic heart disease, with a minimum duration of 1 year according to the hospital discharge report, and patient consent.
In all cases anamneses, physical exams, electrocardiograms and biochemical tests were available. Demographic, anthropometric and clinical characteristics were recorded, along with additional diagnostic tests (echocardiograms, stress tests and coronary angiographies) that were noted in the patients' clinical histories, prescribed treatment, complications from moment of diagnosis to inclusion in the study and hospitalizations during the previous 12 months.
After 6 months of follow-up, mortality and morbidity data (hospital re-admittances) were analyzed according to causation. For the analysis, patients were separated into 2 groups: diagnosed or not with DM at the time of inclusion. To guarantee data quality, an internal audit was performed.
The results of qualitative variables are expressed in absolute values and percentages, and the results of quantitative variables, as mean (standard deviation). To compare the groups, the Student t test was used for parametric variables and the Mann-Whitney U test for non-parametric variables. To determine the significance of the association between qualitative variables, Pearson's c2 test was used.
Survival estimates were calculated using Kaplan-Meier curves, and a log-rank test was used for intergroup comparison.A univariate analysis was performed to establish the factors that predicted cardiovascular events (death and/or admittance), and the statistically significant variables were included in a Cox multivariate analysis using the "forward conditional" method. The Cox model was adjusted using the variables that maintained their significance, as well as age and sex, and the results were expressed as a hazard ratio (HR) with a 95% confidence interval (CI).
SPSS software for Windows, version 15.0, was used for the statistical data analysis. Differences with a probability of type I error below 5% (P<.05) were considered statistically significant.
RESULTS
A total of 1848 patients with ischemic heart disease were screened for the study, 448 patients were excluded because they did not have a hospital discharge report, 279 because informed consent or essential data were missing, and 13 because fewer than 12 months had passed since diagnosis. This meant that 1108 outpatients were recruited with a hospital diagnosis of ischemic heart disease (55% with infarction, 32% with unstable angina and 31% with stable angina).
Diabetes was present in 28.7% and the mean time from diagnosis to inclusion in the study was 7.6 (6) years. There were no significant differences between diabetics and non-diabetics. Sample characteristics, risk factors and comorbidities, additional tests, and patient treatment at the time of diagnosis are presented in Table 1, whereas, Table 2 shows the degree of control of the different risk factors. During the 12 months prior to inclusion, 203 patients (18%) had been admitted for cardiovascular causes, with no differences between diabetics and non-diabetics.
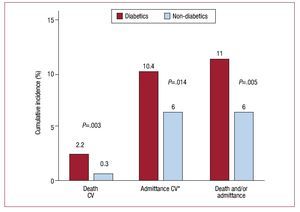
After a mean follow-up of 6.9 (0.9) months, during which 3 patients were lost to follow-up, 15 patients died (1.4%). In Figure 1 it is possible to see mortality and hospitalization rates, as well as their causes. Mortality was significantly higher in the diabetic patient subgroup. This was also the case in the combination of death and hospitalization due to cardiovascular causes. Under multivariate analysis (Figure 2), DM was found to be an independent predictor of cardiovascular events (mortality and/or admittance).
Figure 1. Cumulative incidence of mortality and morbidity in patients included in the CIBAR study. Distribution according to presence of diabetes mellitus. CV: cardiovascular. *Patients that have been hospitalized for cardiovascular causes during follow-up.
Figure 2. Cox regression. Factors determining cardiovascular events (deaths and/or hospitalizations). Adjusted according to age, sex, time since diagnosis, arterial hypertension, diabetes mellitus, heart failure, atrial fibrillation, syncope, abdominal aneurysm, anaemia, coronary surgery, aspirin, oral anticoagulants, angiotensin converting enzyme inhibitors, angiotensin II receptor antagonists, diuretics, nitrates, digitalis, complications and prior hospitalization for cardiovascular causes. CI: confidence interval; CV: cardiovascular; HR: hazard ratio;.
DISCUSSION
Our study population, which is representative of patients with ischemic heart disease, with approximately one third diagnosed with DM, had a relatively benign prognosis. The unfavorable impact of DM on prognosis was confirmed, even on short-term prognosis. Total mortality rate of this group was greater than that of most clinical trials carried out with patients suffering from ischemic heart disease, which is about 1.5% per annum, but these included a much lower percentage of diabetics (12%-17%), and no specific analysis of this subgroup.3
As far as we know, the CIBAR Study describes for the first time in Spain the clinical and epidemiological characteristics and short-term prognosis of a homogeneous cohort of patients with CIC. In addition to being of clinical interest, this study could have certain implications when implementing integrated follow-up strategies between cardiologists and primary care physicians.
Acceptable compliance with clinical practice guides' therapeutic recommendations stands out in the study, with significant differences in treatments with statins and renin-angiotensin-aldosterone system blockers between diabetics and non-diabetics. In spite of this correct compliance, the targets for controlling cardiovascular risk factors were not achieved in a large percentage of patients. In the case of diabetics, only total cholesterol and low density lipoproteins cholesterol (LDL-C) concentrations were controlled better than in the non-DM group. However, there was still a significant residual risk related to dyslipemia (patients with non-controlled LDL-C, high-density lipoproteins cholesterol [HDL-C] and triglycerides). There was little control of blood pressure in these patients and the percentage of diabetics with good glycemia control was low.
The unfavorable influence of DM on prognosis after an acute coronary syndrome4 and also in the case of patients with heart failure5 is known, but there is little data on patients with CIC. In fact the studies carried out in Spain have selected patients after admittance for an acute ischemic event.6-8 In the Euro Heart Survey on Diabetes and the Heart,9 the negative influence of a previous or recent diagnosis of DM was seen after one year's evolution, with a mortality of 7.7% in known diabetics and of 5.5% in recently diagnosed diabetics, in comparison with 2.2% of patients with normal glycaemia, although only 38% had diagnosed CIC.
In the Euro Heart Survey of Stable Angina,10 total annual mortality was 1.5%, and DM was an independent variable for risk of mortality and/or acute myocardial infarction (HR=2.03). Therapeutic compliance, according to the guides' recommendations, significantly improved prognosis.
All the patients included in our study were diagnosed with CIC with more than 1 year's evolution, which was one of the differences from other studies. In spite of the low mortality and morbidity and the fact that most patients were treated according to established indications, a negative impact of DM was seen, which tripled the risk of death over a short follow-up period (7 months), since most deaths in diabetics were due to cardiovascular causes. The difference in hospital admittance due to this cause was also significant, and especially for those due to stroke (2.2% in comparison with 0.5%).
Limitations
Although there was no bias in patient selection and only 3 patients were lost during follow-up, the study population can be considered to be selected since it was chosen by physicians who worked voluntarily. Moreover, the classification into diabetics and nondiabetics was done a posteriori. Furthermore, some data on antidiabetic treatment has not been analyzed and we do not know the dosage of the drugs used, or the degree of therapeutic compliance. These factors could influence the control of different risk factors as well as patient prognosis.
In conclusion, CIC is a condition with a relatively benign prognosis, although some subgroups of patients, such as diabetics, have a worse prognosis, and must be identified to apply stricter treatment controls and risk control targets.
In spite of an acceptable level of knowledge and the application of the recommendations in the guidelines, ideal objectives are attained in a very small percentage of patients.
*The Barbanza Group and CIBAR Study investigators are listed in the appendix.
Correspondence: Dr. F. Otero-Raviña.
Sección de Coordinación Asistencial. Servizo Galego de Saúde. Edificio Administrativo San Lázaro. Santiago de Compostela, A Coruña, Spain
E-mail: fernando.otero.ravina@sergas.es
Received May 16, 2009.
Accepted for publication on September 10, 2009.