Ebstein anomaly (EA) is the most common congenital malformation of the tricuspid valve (TV). Its presentation varies from mild abnormalities with few clinical findings to severe forms that are incompatible with life. The most common associated defect is atrial septal defect, followed by pulmonary stenosis.1 Association with left heart lesions is rare but includes bicuspid aortic valve, noncompacted myocardium, and mitral anomalies.
We present 2 cases of pediatric patients with EA associated with double-orifice mitral valve (DOM) in one and anterior mitral leaflet cleft (MC) in the other, assessed on 2-dimensional and 3-dimensional transthoracic echocardiography (2D-3DTTE). The parents gave informed consent via telephone to publish the cases in an article. To determine the volume of clinical cases of mitral lesions associated with EA in pediatric patients in our institution, we reviewed the electronic archive of examinations performed in the Pediatric Echocardiography Department of the National Institute of Cardiology of Mexico, from January 2012 to December 2019.
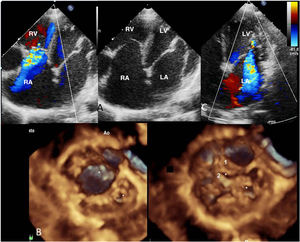
The first case was a 10-year-old boy with a history of palpitations and dyspnea. He was admitted to hospital with a supraventricular tachycardia that was chemically cardioverted. On admission, 2D-3DTTE showed a TV with 40% displacement of the septal leaflet, limited movement of the anterior leaflet, no compromise of the posterior leaflet, and moderate tricuspid regurgitation (figure 1A). Three-dimensional echo of the mitral valve showed a DOM, with a larger 16-mm orifice in a medial position with 2 leaflets: anterior and posterior, with adequate opening; the smaller lateral orifice, in a more apical position, measured 5.7 mm, and had failure of coaptation (figure 1B and video 1 of the supplementary data), with severe regurgitation (figure 1C), and subvalvular apparatus with accessory papillary muscles. Pulmonary systolic pressure was calculated at 38mmHg and ejection fraction was 51%.
TTE images on apical 4-chamber view. A: displacement of the septal leaflet of the tricuspid valve and moderate tricuspid regurgitation on color Doppler. B: 3DTTE reconstruction from the ventricular view; both mitral orifices can be seen in diastole and systole, the larger, medial orifice has 2 leaflets: anterior (1) and posterior (2); the smaller, lateral and more apical leaflet has failure of coaptation. C: severe mitral regurgitation is observed originating at the smaller orifice (video 1 of supplementary data). Ao, aorta; LA, left atrium; LV; left ventricle; RA, right atrium; RV, right ventricle; TTE, transthoracic echocardiogram.
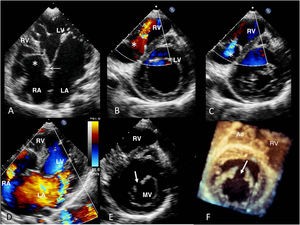
The second case was a 12-year-old girl referred for assessment of supraventricular tachycardia, with 2 previous ablations. 2D-3DTTE showed EA with 50% displacement of the septal leaflet, limited movement of the anterior leaflet, mild regurgitation, a hypertrophic, anatomically small right ventricle (figure 2A-C), patent foramen ovale, and severe mitral regurgitation (figure 2D) caused by the MC, which completely divided the anterior leaflet and ran toward the left ventricular outflow tract, as shown on the 3DTTE images (figure 2E,F and video 2 of the supplementary data). Significant dilatation of the left heart was observed, with ejection fraction of 56% and mean pulmonary artery pressure of 26 mmHg.
TTE on apical 4-chamber view showing displacement of the septal leaflet of the tricuspid valve (A) (black arrow) in relation to the mitral annulus (white arrow) and atrialization of the right ventricle (asterisk), and on parasternal short-axis view in diastole (B), limited movement of the anterior leaflet and displacement of the septal leaflet and mild regurgitation in systole (C). D: severe mitral regurgitation, dilatation of the left atrium, and patent foramen ovale. The 2D parasternal short-axis (E) and the 3D reconstruction from the ventricular surface (F) show the mitral cleft (arrow) that divides the anterior leaflet, running toward the left ventricular outflow tract. See video 2 of the supplementary data. Ao, aorta; LA, left atrium; LV, left ventricle; MV, mitral valve; RA, right atrium; RV, right ventricle; TTE, transthoracic echocardiography. This figure is shown in full color in the electronic version of the article.
Our review of the archives found that, during this period, 25 842 echocardiograms were performed in pediatric patients, as outpatients and inpatients, of which 236 studies from 149 patients had a diagnosis of EA (0.91%). For the analysis of associated lesions, 4 patients with EA in the context of transposition of the great arteries were excluded. We observed a slight male predominance with a ratio of 1.1:1, and a mean age of 8.72±5.3 years. Assessment of severity based on apical displacement of the septal TV leaflet measured on TTE2 showed that 26% corresponded to mild EA, 25% to moderate, and 49% to severe. A total of 82.5% of the patients had at least 1 associated defect; the most common was atrial septal defect, in 117 patients, of whom 78 (54%) had an ostium secundum-type defect (2 of them had partial anomalous pulmonary venous connection) and 39 (27%) had patent foramen ovale, followed by ventricular septal defect in 13 (9%), persistent ductus arteriosus in 10 (7%), pulmonary stenosis in 6 (4%), and pulmonary atresia in 1 (0.7%), all of whom also had atrial septal defects, and 1 had tetralogy of Fallot. The left heart lesions found were bicuspid aortic valve in 1 (0.7%), mitral valve lesions in 11 (7.6%), and noncompacted myocardium in 3 (2%).
The mitral abnormalities found were prolapse with mild regurgitation in 7 patients (1 also had noncompacted myocardium), 2 with mitral dysplasia: 1 with moderate and the other with severe regurgitation, 1 patient with MC, and another with DOM, both with severe mitral regurgitation, which are the cases presented here. The severity of the septal TV leaflet displacement in this group was 1 patient with mild tethering, 5 with moderate, and 5 with severe.
Ebstein's original description mentioned a mild deformity of the mitral valve (MV); however, there are few publications reporting associated mitral abnormalities.3 Gerlis et al.4 described 14 patients with abnormal MV due to valve, chordae, or papillary muscle abnormalities. More recently, Attenhofer Jost et al.5 published a series of 106 patients of whom 39% had left heart abnormalities affecting the myocardium (including systolic or diastolic ventricular dysfunction) and the mitral and aortic valves; the mitral lesions included prolapse in 16 patients and dysplasia in 4.
Lesions of the MV associated with EA such as MC or DOM are uncommon: there is only 1 case report with associated DOM,6 and none with MC. The severity of mitral regurgitation can affect the clinical presentation and patient outcomes in a heart disease that is generally well tolerated in childhood. 3DTTE provides detailed morphology of the TV and associated lesions, and in these cases of the MV, due to the advantage of unconventional views from the left atrium or ventricle.
FUNDINGThis article did not receive any funding.
AUTHORS’ CONTRIBUTIONSC.A. Vázquez Antona contributed to the study conception and design, data analysis and interpretation, writing the article, and approval of the final article for publication. M.R. Álvarez Macedo contributed to obtaining and interpreting data and review and approval of the final version of the article.
CONFLICTS OF INTERESTNone.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2021.01.013