Type A aortic dissection involves high mortality and typically requires surgery. Although it is usually spontaneous, cases have been observed after surgical procedures and, less frequently, interventional procedures.1-3 Due to its low frequency (< 0.1%), there are few data on this topic.1 In 2002, the International Registry of Acute Aortic Dissection (IRAD) reported 26 cases (69% postoperative and 27% due to catheterization) out of a total of 723.1 The epidemiology varied when compared with spontaneous presentations: those with iatrogenic aortic dissection were older, were more frequently diabetic or hypertensive, and had a greater degree of atherosclerosis, or a history of coronary bypass. Symptoms also varied: patients with iatrogenic dissection had less back pain or, when present, it had different characteristics, a higher frequency of hypotension and shock, and a high probability of ischemia and myocardial infarction (36% and 15%, respectively).
Although the prognosis of iatrogenic presentations was associated with high mortality in the past,1 recent registries, such as the German GERAADA, indicate a mortality rate that is similar to spontaneous dissection.2
Our objective was to analyze the incidence, characteristics, and prognosis of iatrogenic aortic dissection following catheterization.
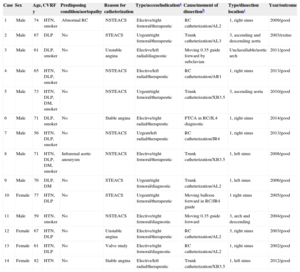
Between October 2000 and July 2014, we performed 58 518 procedures, 36 372 of which were diagnostic and the remaining 22 146 were therapeutic. We identified 14 patients with dissection of the descending aorta/arch, without coronary dissection. The incidence was 0.02%, with a mean age of 68.5 years and a predominance of men (Table). The main reason for catheterization was chest pain along with acute coronary syndrome (10 cases). Five patients were treated urgently, 3 of whom had ST elevation. In 4 patients, the procedure was exclusively diagnostic, while 7 patients underwent successful coronary intervention. Guiding catheters were used in 10 patients, but the intervention had to be postponed due to the dissection. The approaches used were as follows: right femoral artery in 9 patients (64.3%), left radial in 4, and right radial in 1. All the radial approaches were performed from 2011 onward. The average contrast amount was 241 mL, fluoroscopy time was 26.3 minutes, and total time was 89.3 minutes. Presentation was acute in all patients and coincided with the catheterization of a vessel in 10 patients. In general, dissection occurred with 6-Fr catheters (Amplatz in 6 patients, extrabackup in 3, and Judkins in 3) and 2 with the 0.35″ guide. Twelve patients received acetylsalicylic acid, 4 in conjunction with clopidogrel, and 1 in addition to fibrinolysis with tenecteplase. All patients received anticoagulants during the procedure.
Individualized Summary for Each of the Patients
| Case | Sex | Age, y | CVRF | Predisposing condition/aortopathy | Reason for catheterization | Type/access/indicationa | Cause/moment of dissectionb | Type/dissection locationc | Year/outcome |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Male | 74 | HTN, smoker | Abnormal RC | NSTEACS | Elective/right femoral/therapeutic | RC catheterization/AL2 | 1, right sinus | 2009/good |
| 2 | Male | 67 | DLP | No | STEACS | Urgent/right femoral/therapeutic | Trunk catheterization/AL3 | 3, ascending and descending aorta | 2003/exitus |
| 3 | Male | 61 | DLP, smoker | No | Unstable angina | Elective/left radial/diagnostic | Moving 0.35 guide forward by subclavian | Unclassifiable/aortic arch | 2011/good |
| 4 | Male | 65 | HTN, DLP, smoker | No | NSTEACS | Elective/left radial/therapeutic | RC catheterization/AR1 | 1, right sinus | 2013/good |
| 5 | Male | 73 | HTN, DLP, DM, smoker | No | NSTEACS | Urgent/right femoral/therapeutic | Trunk catheterization/XB3.5 | 3, ascending aorta | 2010/good |
| 6 | Male | 71 | DLP, smoker | No | Stable angina | Elective/right radial/therapeutic | PTCA in RC/JL4 diagnostic | 1, right sinus | 2014/good |
| 7 | Male | 56 | HTN, DLP, smoker | No | NSTEACS | Urgent/left radial/therapeutic | RC catheterization/JR4 | 1, right sinus | 2013/good |
| 8 | Male | 71 | HTN, DLP, DM, smoker | Infrarenal aortic aneurysm | NSTEACS | Elective/right femoral/therapeutic | Trunk catheterization/XB3.5 | 1, left sinus | 2008/good |
| 9 | Male | 76 | DLP, DM | No | STEACS | Urgent/right femoral/diagnostic | Trunk catheterization/AL2 | 1, left sinus | 2006/good |
| 10 | Female | 77 | HTN, DLP | No | STEACS | Urgent/right femoral/therapeutic | Moving balloon forward in RC/JR4 guide | 1 right sinus | 2005/good |
| 11 | Male | 59 | HTN, smoker | No | NSTEACS | Elective/right femoral/diagnostic | Moving 0.35 guide forward | 3, arch and descending | 2004/good |
| 12 | Female | 67 | HTN, DLP | No | Unstable angina | Elective/right femoral/therapeutic | RC catheterization/AL2 | 3, right sinus | 2003/good |
| 13 | Female | 61 | HTN, DLP | No | Valve study | Elective/right femoral/diagnostic | RC catheterization/AL2 | 1, right sinus | 2002/good |
| 14 | Female | 82 | HTN | No | Stable angina | Elective/left radial/therapeutic | Trunk catheterization/XB3.5 | 1, left sinus | 2012/good |
PTCA, percutaneous angioplasty; AL, Amplatz catheter, left coronary; AR, Amplatz catheter, right coronary; RC, right coronary; DLP, dyslipidemia; DM, diabetes mellitus; CVRF, cardiovascular risk factors; HTN, hypertension; JL, Judkins catheter, left coronary; JR, Judkins catheter, right coronary; STEACS, ST-elevation acute coronary syndrome; NSTEACS, non-ST-elevation acute coronary syndrome; XB, extra-backup catheter (“high support” for left coronary; all are guides).
During a mean follow-up of 62.4 months, there was 1 hospital death. None of the other patients who had been treated conservatively developed complications secondary to dissection, progression, ischemia, pain, or recurrence (Table).
There are few data on this complication, and published articles are limited to small case series or case reports. In addition, most include dissections of the ascending aorta and those occurring after dissection in a coronary artery.3,4 Here, we have excluded this type because the access port is different. In the coronary arteries, conservative management has been described with good results if the vessel continues to have good flow and the dissection is small4; if not, implanting a stent at this point would seal the flap and would generally resolve the problem satisfactorily.3,4 In 2002, Dunning et al3 published a series of 9 patients with coronary dissection extending to the aorta (incidence, 0.02%) and proposed a classification in 3 grades: type 1, dissection limited to the sinuses of Valsalva; type 2, dissection of the ascending aorta outside of the sinuses < 4 cm; and type 3, dissection ≥ 4 cm. These authors proposed that stent implantation was sufficient in the limited forms, but those with type 3 required surgery.3
Our series is different since coronary intervention does not resolve the complication. Furthermore, indicating complex surgery of the ascending aorta could be catastrophic in patients who are often under the effects of intense antithrombotic treatment and have had a recent myocardial infarction.1–4 It is therefore a relevant complication considering the volume of procedures performed in our setting.5
After following-up, our patients for more than 5 years on average, we have seen excellent outcomes, regardless of the access used (radial or femoral), even though many continued to receive intense antithrombotic treatment when their condition was acute. The profile of the patients affected with this complication is that of a male in his sixties, with cardiovascular risk factors (mainly atherosclerotic-ischemic), who undergoes a complex procedure (generally therapeutic) with difficult coronary catheterization.
Based on this information, we can conclude that if there are no important symptoms, the dissection is small and the imaging studies show no progression (Figure), it seems reasonable to follow a conservative strategy. If not, surgery may need to be considered.
Patient number 5 (Table). Arrow: Dissection; A: Acute moment, which required cessation of the procedure; B: 3 days later, aortogram showing definite improvement; at that time, angioplasty was done in the anterior descending artery without complications; C: Tomography showing the initial hematoma/thrombotic dissection at the ascending aorta (A); D: Follow-up tomography 9 months later (at the same height of C) showing complete symptom resolution.