The transradial approach is the approach of choice in many centers for its advantages over the femoral approach; however, in up to 12% of procedures, the radial artery is occluded,1,2 which forces using alternative routes. Traditionally, the transulnar approach has been considered contraindicated in cases with a positive Allen test and/or evidence of ipsilateral radial occlusion, because of the risk of inducing acute hand ischemia. Recently published studies indicate this strategy seems to be safe in the short term.3,4 However, we do not know how the hand can be vascularized under these circumstances or its long-term outcome.
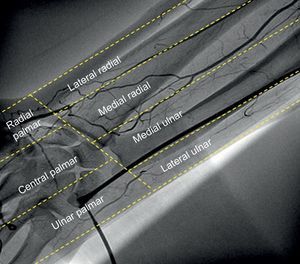
From January 2009 until February 2013, we studied hand vascularization in 14 patients, applying our transulnar approach protocol, which includes an angiography (10mL to 3ms/s) of the forearm, and we recorded 1 ipsilateral radial occlusion. To systematize the forearm vascularization, we divided it into 4 regions according to their relationship with the radial, ulnar, and interosseous arteries: lateral radial, medial radial, medial ulnar, and side ulnar regions. We subdivided the vascularization of the palmar arch into 3 regions separated by the second and fourth metacarpal bones: radial palmar, central palmar, and ulnar palmar regions (Figure). In addition, we conducted long-term follow-up on these patients, assessing the occurrence of hand sensory disorders, pain, or mobility problems. In a subgroup (the last 7 patients in the series), ultrasound follow-up was performed to assess ulnar artery permeability.
Using angiography of the forearm, we were able to show that these patients had simultaneous occlusion of the ulnar and ipsilateral radial arteries (ulnar occlusion was acute due to the arterial sheath covering the entire lumen). Despite having both arteries occluded, patients suffered no symptoms or signs of acute hand ischemia during the procedure, because the palmar arch was vascularized through small collateral branches, all from the interosseous artery. In 12 patients, we observed collateral branches over a region of the forearm and/or palmar arch. More often (11 cases), they led to the radial artery (distal to the occlusion) in the medial area, with direct insertion to the palmar arch (palmar-ulnar region, 10 cases). The table shows all the collateral branch insertions in the 14 cases. After an average follow-up of 26 [interquartile range, 10 to 43] months, all patients retained ulnar pulse. There was no evidence of chronic ischemia or signs of serious effects on the ulnar nerve (motor and sensory). No claudication or pain was observed in any of the patients after they conducted a series of hand openings and closings. Ulnar artery permeability was recorded for all patients in the ultrasound follow-up subgroup.
With the above-described findings, it can be inferred that the absence of acute hand ischemia in the transulnar approach with ipsilateral radial occlusion may be due to the presence of collateral branches from the interosseous artery, which in most patients led to more than one region of their hands. Because we observed collateral branches going to the vascularized region due to the ulnar artery in 11 of 14 patients, we considered that the recruitment of these collateral branches was acute. This rapid recruitment would explain the shortage of published cases of acute hand ischemia following arterial catheterization through forearm arteries. Despite the very long-term safety demonstrated in our series, and due to the theoretical possibility of ulnar artery occlusion after the procedure, we recommend caution in using this route in case of ipsilateral radial occlusion.
CONFLICTS OF INTERESTRamón Rodríguez-Olivares receives a joint grant from European Association of Percutaneous Cardiovascular Interventions (EAPCI) and Edwards Lifesciences.