Keywords
Interatrial communication (IAC) is the fourth most frequently encountered congenital heart malformation, and one of the most common in adults.1,2 As an alternative to surgical closure of ostium secundum, percutaneous closure procedures have been developed,3 with the aim of avoiding sternotomy and coronary bypass, thus reducing morbidity and length of hospital stay. Multiple devices have been developed, and the most recent of these, the auto-expandable Amplatzer device, seems to have the best properties with regard to safety and efficacy. Transient ST segment elevation in the inferior derivations during device implantation has been anecdotally reported (1 case in a series of 100 cases).4
In our experience with closure of IAC in adults with the Amplatzer device, we observed that ST segment elevation occurred much more frequently (6 out of 8 cases). We present these cases and develop a brief discussion concerning this finding.
CLINICAL CASES
From December 2000 to May 2001, 8 adults diagnosed with IAC ostium secundum and the need for its correction, with an average age of 49±15 years (range 23 to 69 years) underwent percutaneous closure with the Amplatzer device. Patient characteristics are listed in Table 1. In all patients a transesophageal echocardiogram (TEE) was performed to define the morphology and diameter of the defect. The conditions required were: ostium secundum IAC, maximum 30 mm diameter with a free border greater than 5 mm. The implant was performed under general anesthesia in all cases. The choice of the device was based on the size as defined by TEE and that provided by a balloon occluder. The procedure was carried out following the usual protocol described previously.5-10 We were particularly careful with the introduction of the device into the sheath, which was performed under physiologic saline serum, and we performed the operation repeatedly until we were sure that no bubbles appeared in the serum upon extraction.
During the manipulation and implantation of the device in 6 of the 8 cases a transitory (<1-2 minutes) but significant elevation of the ST segment was observed in the inferior derivations (Figure 1). This elevation was variable in magnitude; in 2 cases it was greater than 3 mm and in the remaining 6 cases 1 to 3 mm, and was not associated with changes in arterial pressure, cardiac frequency, or arterial oxygen saturation, and, obviously, symptoms were not present as the patient was anesthetized.
Fig. 1. Electrocardiography monitor recording that shows the ST segment elevation in derivations II and III.
In the first case in which we observed a marked ST segment elevation (case 2, 59-year-old woman) we performed coronary angiography, which revealed a significant lesion in the right proximal coronary artery. This was evaluated by intracoronary echography, which revealed a minimum luminal area of 3.5 mm², and we decided to treat the lesion with angioplasty. In the immediately preceding cases (younger patients), we also observed changes in the ST segment, but coronary angiography was not considered appropriate. In cases 7 and 8, the patients´ age, coronary angiography had been performed previously, and was normal.
We did not observe changes in any patient on electrocardiogram performed after the procedure. We also did not observe changes in the segmental contractility of the left ventricle on echocardiogram.
DISCUSSION
The transitory elevation of the ST segment in the inferior derivations has been described as a rare complication during the percutaneous closure of IAC with the Amplatzer device, and it has been attributed to the possible embolization of small air bubbles.4 This complication has been observed more frequently during other non-coronary percutaneous procedures, specifically mitral valvuloplasty (MVVP) with Inoue balloon. Vahanian et al11 described this finding in 2.6% of MVVP procedures; it was observed upon deflating the balloon, and attributed it to air embolisms introduced into the right coronary artery, given the high location of the right coronary ostium in relation to the left in the decubitus supine position. In all cases, right coronary angiography was normal. Ludman et al12 described this complication in a greater percentage of valvuloplasties (7.4%), observing the elevation immediately before the balloon traversed the mitral valve, so that they considered it unlikely that an air embolism was the cause. These authors postulated the possible existence of ischemic or mechanical changes, or both (coronary spasm, deformation of the AV furrow, etc.) caused by the manipulation of rigid catheters within the atria. As an alternative explanation, they proposed the possible embolization of small thrombi from the atrial wall, but the clinical picture associated with this complication is distinct from the transitory ST segment elevation observed.
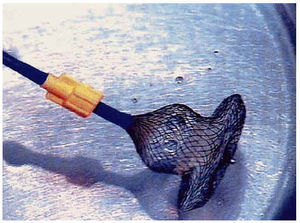
In our series, transitory ST segment elevation in inferior derivations was frequently observed (in 6 of 8 cases). Initially, we thought this was due to an air embolus, and for this reason we were very careful in subsequent cases during the process of introducing the device into the sheath (Figure 2). The special care taken, together with the observation that the inadvertent injection of small air bubbles during coronary angiography produces infrequent electrocardiographic changes, makes us doubt that this etiology is the cause in all cases.
Fig. 2. Liberation of bubbles upon extracting the device from the sheath after the first introduction of same.
In the second case where the elevation was observed (in a 59-year-old woman), coronary angiography showed a significant lesion in the right coronary artery, without a clear causal lesion-ST segment change relationship. In the following cases in which we observed an ST segment elevation, young patients or older patients with normal coronary angiography were involved. Therefore, an alternative explanation to the air embolus would be the concurrence of transitory changes in the vasomotor tone and mechanical deformities of the AV furrow, or both, caused by the manipulation of the devices within the atria, causing compromise of the right coronary fluid.
The fact that this complication has only been communicated anecdotally could be explained by: a) very brief changes in ST segment time that could be imperceptible if they were not specifically being studied, and b) the published series are for the most part made up of children and young adults, in whom this finding is probably less frequent. Our series basically consists of adults, and the 6 patients in whom we observed the change were more than 46 years old. The greater size of the sheaths and devices in adults could influence these findings.
In any case, whatever the etiological mechanism, the only avoidable factor is the embolization of air, so that it is important to be very careful with the external manipulation of the device, checking several times that there are no air bubbles.
Correspondence: Dr. J.M. de la Torre Hernández.
Unidad de Hemodinámica. Hospital Marqués de Valdecilla.
Avda. Valdecilla, s/n. 39008 Santander. Spain.
Correo electrónico: chematorre@mundivia.es