Mitral regurgitation (MR) is the second most common valvulopathy in Europe and has a poor prognosis despite medical treatment, yet many patients with this condition have significant comorbidities, leading to a prohibitively high surgical risk.
The MitraClip percutaneous repair device (Abbott Laboratories, USA) has been established as a safe and effective option for the treatment of patients with high surgical risk and severe symptomatic MR despite optimal medical treatment.1
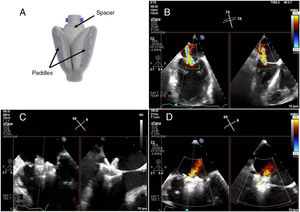
Recently, reasonable initial results have been reported2,3 with the PASCAL percutaneous mitral repair device (Edwards Lifesciences, USA), and in February 2019 it received the CE mark for the treatment of degenerative or functional severe MR. This device expands the therapeutic arsenal for transcatheter mitral repair by offering the following features: a) broad (approximately 25 mm), convex paddles; b) a central spacer (10mm) that occupies the regurgitant orifice—the combination of which increases coaptation and reduces leaflet stress; c) the option of elongation that allows safe maneuvering in the subvalvular space; and d) the possibility of individual leaflet capture in complex anatomies (figure 1A).
A: PASCAL device in a closed position showing the broad paddles and central spacer. B: X-plane color Doppler of the mitral valve on transesophageal echocardiography (TEE) prior to implantation. C: individual capture of the posterior leaflet. D: X-plane color Doppler of the final mitral valve. Reproduced with permission from Edwards Lifesciences (USA).
We present the first 2 cases in Spain of percutaneous mitral repair using the PASCAL device in patients with functional and degenerative MR, respectively.
The first patient was a 76-year-old man who had idiopathic dilated cardiomyopathy with moderate biventricular dysfunction, severe functional MR and severe tricuspid regurgitation due to annular dilatation and pacemaker lead interference. He was in New York Heart Association (NYHA) functional class III and had chronic renal failure with a baseline glomerular filtration rate of 20-25mL/min. As surgery was contraindicated due to his level of comorbidity, it was decided to perform percutaneous repair with the PASCAL device. Transthoracic echocardiography showed severe functional MR due to central (A2-P2) tenting, which was more pronounced at the posterior leaflet (Carpentier IIIb), causing marked attenuation of systolic flow in the pulmonary veins (figure 1B).
Under general anesthetic and transesophageal echocardiographic guidance, a first device was implanted centrally, which reduced the regurgitation grade to III/IV with a persistent residual jet posteromedially with no stenosis.
It was decided to implant a second device, adjacent and medial to the first device. Several attempts were made at simultaneous capture, but the significant posterior jet persisted, so it was decided to optimize posterior leaflet capture by clasping the leaflet individually (figure 1C). After implantation of the second device, the MR grade was reduced to II/IV with a final V wave of 17 mmHg (35 mmHg initially), a clear improvement in the flow pattern in the pulmonary veins and a final mean gradient of 2 mmHg (figure 1D). At follow-up, there was an improvement in signs of congestion and a significant reduction in N-terminal pro-brain natriuretic peptide (NT-proBNP) (21 727 initially; 2894 at discharge).
The second patient was an 84-year-old woman in NYHA III-IV with severe degenerative MR secondary to posterior leaflet flail (P2 scallop), showing cord rupture at this level and marked indentation between P1 and P2 with reverse systolic flow in the pulmonary veins and a nondilated left ventricle with preserved ejection fraction (figure 2a). Given her advanced age, the multidisciplinary team decided percutaneous mitral repair would be suitable.
The procedure was carried out under general anesthetic and transesophageal echocardiographic guidance. A first PASCAL device was positioned centrally, but after capture there was a significant residual regurgitant jet, so it was decided not to deploy the device but to opt for a double-implant strategy.
One PASCAL device was implanted uneventfully in a medial position and a second PASCAL was implanted lateral and adjacent to the first, allowing optimized unilateral capture of the posterior leaflet (figure 2B). Finally, it was possible to reduce the regurgitation to grade II/IV with near normalization of the flow pattern in the pulmonary veins and a V wave in the left atrium of 18 mmHg (55 mmHg initially) with a final transvalvular gradient of 5 mmHg. Transthoracic echocardiography prior to discharge confirmed the stability of the devices and the persistent reduction in MR grade (figure 2C).
Neither of the 2 patients had procedure-associated complications.
These are the first 2 cases of percutaneous mitral valve repair with the PASCAL device in Spain in patients with functional or degenerative MR. In the first patient, after several attempts at simultaneous capture of both leaflets that failed to reduce the posterior jet, the device allowed individual capture of the posterior leaflet to significantly reduce the residual jet. In the second patient, given the valve anatomy with prolapse and marked central indentation of the posterior leaflet, the option of individual capture facilitated the procedure and the final outcome.
Although the PASCAL device is a relatively new tool in our setting, in both cases, the procedure time did not exceed the usual time for a repair with the MitraClip system due to the similarity between the 2 in terms of implantation technique. However, because of the features of this device, it generates more artefact on echocardiography, which interferes with visualization and procedural guidance on transesophageal echocardiography.
Currently, there are no medium-to-long-term results for percutaneous mitral repair using this device. However, its features described above provide greater versatility in the treatment of patients with complex mitral anatomy.