Keywords
INTRODUCTION
Sinus Valsalva aneurysms are usually congenital defects, with prevalence in males and oriental population.1 The cause of their appearance is an incomplete fusion of the distal bulbar septum that divides the pulmonary artery and the aorta and attaches to the annulus fibrosus of the aortic valve. There is also thinning of the aortic media observed in affected sinus which can progressively dilate over time, especially in cases of arterial hypertension.2 Although Valsalva aneurysms may involve all 3 sinuses, more frequently the right and noncoronary are involved. During rupture they open most frequently to the right ventricle or right atrium. The left sinus is not derived embriologically from bulbar septum and therefore is rarely affected by congenital lesions. This anomaly can be unrecognized for many years. Only rarely, in cases of major aneurysm, do they cause a-v block, aortic incompetence or subvalvular pulmonary stenosis.3,4 Symptoms usually appear when the aneurysm ruptures into a cardiac chamber causing continuous murmur, excercise intolerance, symptomatic heart failure, or sudden death, depending on the magnitude of left to right shunt. Traditional treatment is surgical excision and patch closure in cardiopulmonary bypass.5
Percutaneous closure of ruptured sinus Valsalva aneurysm (RSVA) was first attempted by Cullen et al6 in 1994 using a Rashkind umbrella. Since then a few reports have been published with the use of different available closure devices.7-10 We would like to share our experience in transcatheter closure of 6 RSVA in 5 patients.
METHODS
From March 2007 to January 2008 5 patients (mean age, 33.2 y) underwent transcatheter closure of RSVA. Their clinical data are presented in the Table. The observed symptoms were as follows: dyspnoea, orthopnea, chest pain, palpitations, and syncope. In 4 patients there was congenital RSVA. One of them (Table, patient 2) underwent surgical closure of RSVA one year before this procedure. Another patient (Table, 3) probably had iatrogenic RSVA, from left coronary sinus into the right pulmonary artery, after surgical tetralogy of Fallot (TOF) correction. In all patients the diagnosis was established after detailed clinical and echocardiographic examination. Angio 64 multislice computed tomography (CT) was also performed prior to the procedure for better visualization of location of the shunt and for measurements. All patients were informed about two methods of treatment—cardiosurgery and the relatively new option, transcatheter closure. All prefered transcatheter closure of RSVA and signed informed consent.
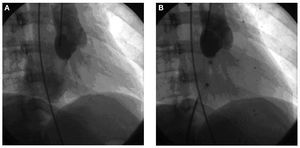
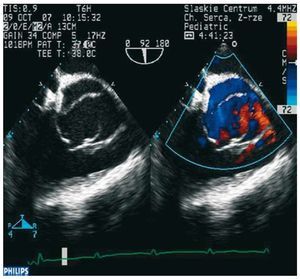
The procedures were carried out under general anesthesia with both fluoroscopy and transoesophageal in right anterior oblique (30 degree), postero-anterior or left anterior oblique (70 degree) projection, depending on best visualization of shunt (Figure 1A). The diameter of the RSVA was assessed on the basis of angiography and CT (both were equal in each case). Then a right Judkins coronary catheter was introduced with the use of Terumo wire from the aorta through the ruptured sinus to the right atrium or pulmonary artery, and Terumo wire was exchanged for 0.035 inch/260 cm long Amplatz extrastiff guide wire. This wire was snared and taken out with Lasso (Microvena) introduced from the femoral vein (arteriovenous loop was created). Over the wire a 7 or 8 F transseptal AGA sheath (45 or 180 deg) was introduced from femoral vein through the ruptured sinus to the ascending aorta. Amplatzer Duct Occluder (ADO) or Amplatzer Atrial Septal Occluder (ASO) (both AGA Medical Corp., Plymouth, MN, USA) were applied. They were chosen according to RSVA morphology - equal or up to 5 mm larger than RVSA orifice diameter. Stability of the opened device was confirmed during "Minnesota wiggle" (gentle pulling and pushing of the delivery system). Once the position of the device was considered acceptable, ECG was analyzed and Amplatzer device was released. The TEE and aortography then repeated (Figures 1B and 2).
Figure 1. A: aortography; opacification of the right atrium through ruptured Valsalva sinus aneurysym. B: aortography; proper position of device.
Figure 2.Echocardiography; proper position of device.
RESULTS
The procedures were successful in all cases, but finished in 4 patients. In and 18 y old female (Table, 3) with postsurgical left coronary sinus to pulmonary artery communication, after deployment of the device changes in ECG appeared (ST depression) and the device still connected with the delivery system was withdrawn. In patient number 4 (Table), 8/6 ADO was initially implanted, but went through the RSVA into RA. The procedure was started once again from the beginning and 6 mm ASO was implanted without complication. In another patient, after closure of recanalized postsurgical RSVA (Table, 2) the second defect was echocardiographic (TEE) guidance. After canulation of the femoral artery and vein a 6F vascular sheath was introduced. Diagnostic catheterization was performed. Then the shunt was visualized during aortography with a Pigtail 6F catheter placed just above the aortic valve recognized after closure of the first one. This second defect was closed with 10/8 mm ADO during another catheterization after 6 months, with good final result. After the procedure, patients received aspirin 3-5 mg/kg for 6 months. One complication was observed - arteriovenous fistula in the groin after the second procedure (Table, patient 2) which needed vascular surgical intervention. In patient number 1 (Table), trivial residual shunt was diagnosed in TTE before discharge home. Complete closure was, however, confirmed in all patients during the first out-patient visit after 1 month. All patients were followed up by TTE with Doppler and color flow imaging after 1, 3, 6, and 12 months and every 6 months. The follow-up range was 9-19 months. No complications were observed during that time.
DISCUSSION
Sinus Valsalva aneurysm are usually congenital and involve right- or noncoronary sinus. Symptoms appear after rupture of aneurysm into a heart chamber. Aneurysm rupture happens usually in adulthood. It may follow strenuous effort, infection or trauma. In the oldest patient from our group (51-year-old male) the first symptoms appeared during infection. Another predisposing factor for rupture is arterial hypertension. In our group, arterial hypertension was observed in 3 patients. RSVA can appear as acquired malformation, as was observed in one young woman after surgical correction of TOF, and was considered as iatrogenic. Other causes of acquired RSVA can be aortic valve replacement, infective endarteritis, tuberculosis, syphilis or mechanical injury such as a car accident.11
The severity of symptoms depends on magnitude of the left to right shunt. The diagnosis is established during echocardiographic examination with color-Doppler, which shows affected sinus and the chamber the shunt is directed to. Our experience confirms the usefulness of multisliced angio-CT. On the basis of this examination, precise morphology of RSVA and the size of opening was measured, which was equal to that achieved during angiography. During the procedure TEE was a very helpful diagnostic tool that could confirm proper device placement and assess the function of the aortic valve and the presence of eventual residual shunt. Control aortography as well as observation of eventual changes in ECG must be performed before unscrewing of the device. In our patient with iatrogenic left sinus Valsalva aneurysm ruptured into the pulmonary artery, ST depression appeared in ECG after device deployment (still attached to delivery system). The device was withdrawn and the procedure abandoned.
Surgical closure of RSVA in cardiopulmonary bypass was the only possible treatment with relatively low perioperative risk (mortality <2%) in the past.5 Progress in interventional cardiology during recent years and especially introduction of Amplatzer devices to clinical use enable closure of many undesirable vascular connections. For transcatheter closure of RSVA, initially Rashkind umbrella6 and coils8 were used. However, coils can be implanted only in cases of minor connections. The effectiveness and safety of ASO and ADO in transcatheter closure of RSVA and other undesirable vascular connections was confirmed previously.7,9,10,12,13 In case of RSVA when ADO has unstable position, application of ASO can be a better solution due to its bigger retention discs. Using transcatheter closure can avoid possible complications of medial sternotomy and cardiopulmonary bypass. Reduced pain for the patient, absence of surgical scar, shorter hospitalization and convalescence time are also important advantages. Transcatheter treatment may be especially useful in the case of recanalisation after previous surgical treatment, when the risk of reoperation is substantially higher. The limitation of the study is a short period of follow-up. Theoretically there exists the risk of repeated rupture of the sinus of Valsalva, because of the presence of abnormal tissue. On the other hand, epithelialization of the device can make surrounding tissue stronger. These questions remain unanswered; therefore, longer follow-up after such procedures is needed. In conclusion, percutaneous closure of ruptured sinus Valsalva aneurysm is a feasible procedure that can replace surgical treatment.
Correspondence: Dr J. Bialkowski,
Silesian Centre for Heart Diseases,
Ul. Szpitalna 2; 41-800 Zabrze, Poland
E-mail: jabi_med@poczta.onet.pl
Received December 3, 2008.
Accepted for publication February 11, 2009.