Keywords
INTRODUCTION
Hypertension (HT) is one of the risk factors for coronary artery disease and left ventricular hypertrophy (LVH). Different studies have shown that the concentration of the N-terminal fragment of B-type natriuretic peptide (NT-proBNP) in serum is increased in hypertensive patients with LVH.1 However, the urinary concentrations of NT-proBNP in cases of essential HT have not been analyzed. Moreover, there are few previous studies on the presence of natriuretic peptides in urine and their clinical implications.2,3
We hypothesized that NT-proBNP could be detected in the urine of patients diagnosed as having HT, and that the presence of LVH could be related to the increase in the urinary concentration of this peptide. The objective of this study was to evaluate the predictive power for the diagnosis of LVH in a group of patients with essential HT but no symptoms of heart disease.
METHODS
In this cross-sectional study, we analyzed 160 hypertensive patients with no cardiologic symptoms (age, 61 [14] years; 53% men). Their arterial blood pressure was taken between 8:00 and 11:00 AM, and HT was diagnosed in accordance with the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. All the patients were receiving stable medical treatment. Patients with secondary HT, an ejection fraction (EF) less than 50%, ischemic heart disease, dilated cardiomyopathy, continuous arrhythmia, more than mild valve failure, chronic or acute renal or liver disease, immunologic diseases, human immunodeficiency virus, alcoholism, and/ or drug addiction were excluded. The control group consisted of 32 subjects who had normal arterial blood pressure measurements and normal results on Doppler echocardiography, electrocardiography, blood cell count and other laboratory tests. The study was performed in agreement with the good clinical practice guidelines and the ethical standards for human experimentation established by the Declaration of Helsinki.
The serum and urinary concentrations of NT-proBNP were determined using an electrochemiluminescence immunoassay (Cobas 6000 E-601, Roche Diagnostics, Germany). The results were expressed in pg/mL, the minimum detection limit was 5 pg/mL and recovery was 97%. The coefficient of total variation was 2.6% for the analysis of serum NT-proBNP and 3.2% for NT-proBNP in urine in our group of patients.
The 2-dimensional images, Doppler spectrum and color Doppler were analyzed using a computerized system (Eco-Dat; Software Medicina, SL). Left ventricular mass was measured using the Devereux formula and, in this study, we utilized a sex-specific criterion for the diagnosis of hypertrophy.4
The continuous variables were expressed as the mean plus or minus the standard deviation or as the median [interquartile interval] for NT-proBNP, and as the percentage for the categorical variables. The normal distribution of the variables was studied using the Kolmogorov-Smirnov test. The NT-proBNP concentrations were compared by means of the Mann-Whitney test, and they were logarithmically transformed to correlate the values in serum and urine and perform multiple linear regression analysis with urinary NT-proBNP/creatinine as a dependent variable. The diagnostic power of the urinary NT-proBNP level for the presence of hypertrophy was analyzed using a receiver operating characteristic (ROC) curve. Finally, logistic regression was performed to determine whether the urinary NT-proBNP/ creatinine ratio was an independent predictor of LVH. The threshold of statistical significance was considered to be a P value less than .05. The SPSS 11.5 statistical software package (SPSS, Inc., Chicago, Illinois, USA) was employed.
RESULTS
Table 1 shows the characteristics of our hypertensive patients with (n=60) and without LVH (n=100). The serum and urinary NT-proBNP concentrations (with or without normalization for creatinine) were higher in the patients with LVH as compared with the group in which there was no LVH (P<.0001) and with the control group (P<.0001). However, the levels of NT-proBNP in serum and urine (with or without normalization) were similar in the group without LVH and the controls (Table 2).
The serum NT-proBNP concentrations were correlated with those of the peptide in urine when normalized for creatinine (r=0.49; P<.0001) and without normalization (r=0.50; P<.0001). Moreover, the urinary levels of NT-proBNP/creatinine were correlated with the left ventricular mass index (LVMI) (r=0.34; P<.0001). Multiple linear regression analysis was also carried out to determine whether age, sex, systolic arterial pressure, time elapsed since onset of HT, the ratio of the early peak transmitral flow velocity (E wave) to the late peak transmitral flow maximal velocity (A wave) (E/A) in diastole, LVMI, treatment, and/or serum NT-proBNP influenced the urinary NT-proBNP values. Age (P=.034) and LVMI (P=.026) were identified in model 1 and in model 2 (model 1 plus serum NT-proBNP), the only predictive factor identified was the serum NT-proBNP concentration (P=.001).
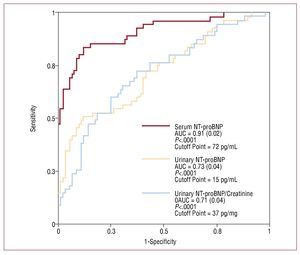
Upon analysis of the utility of urinary NT-proBNP/creatinine to detect LVH using a ROC curve, an area under the curve (AUC) equal to 0.71 was obtained (P<.0001), with an optimum cutoff point of 37 pg/mg (sensitivity, 53%; specificity, 85%; positive predictive value [PPV], 67%; and negative predictive value [NPV], 74%), whereas for non-normalized urinary NT-proBNP, the AUC was equal to 0.73 (P<.0001), with a cutoff point of 15 pg/mL (sensitivity, 53%; specificity, 85%; PPV, 67%; and NPV, 75%) (Figure). The NT-proBNP levels in serum obtained an AUC equal to 0.91 (P<.0001), with a cutoff point of 72 pg/mL (sensitivity, 85%; specificity, 85%, PPV, 77%; and NPV, 90%).
Figure.Receiver operating characteristic (ROC) curves for the detection of left ventricular hypertrophy based on the serum and urinary concentrations of the N-terminal fragment of B-type natriuretic peptide (NT-proBNP) in subjects with essential hypertension. AUC indicates area under the curve.
Finally, when we performed logistic regression analysis to identify the predictors of LVH, we demonstrated that age (odds ratio [OR] = 1.118; 95% confidence interval [CI], 1.068-1.179; P<.0001), urinary NT-proBNP/creatinine values greater than 37 pg/mg (OR=4.074; 95% CI, 1.523-10.89; P=.009) and serum NT-proBNP levels greater than 72 pg/mL (OR=18.21; 95% CI, 6-55; P<.0001) were independent predictors of LVH. The remaining variables (systolic arterial pressure, sex, obesity and time elapsed since onset of HT) did not reach statistical significance.
DISCUSSION
The serum NT-proBNP concentration is a powerful marker for left ventricular hypertrophy and dysfunction,5,6 but the number of studies performed in patients with essential HT is limited.7 On the other hand, the calculation of the value of the level of this peptide in urine, previously demonstrated in heart failure, has not been determined in patients with HT. In this study, we have calculated, for the first time, the urinary concentrations of NT-proBNP in patients diagnosed as having essential HT and its capacity for predicting LVH.
Some reports have demonstrated a relationship between an increase in left ventricular mass and the serum NT-proBNP concentration in hypertensive patients.8 In our study, the patients with LVH had higher levels of this peptide in serum and urine, although there were no significant differences when the hypertensive patients without LVH and the control group were compared. Moreover, the urinary concentrations were correlated with the LVMI.
On the other hand, we obtained a good and statistically significant correlation between the serum and urinary levels of NT-proBNP with or without normalization for creatinine. The urinary concentration of NT-proBNP would reflect renal synthesis of this peptide and the quantity produced in and filtered from the myocardium. Moreover, multiple linear regression analysis identified age, LVMI and serum BT-proBNP levels as independent predictors of the urinary concentrations of this marker. These results can be extrapolated to others obtained previously, in which the influence of these factors has been observed.3,7,8 Moreover, the urinary NT-proBNP values, normalized for creatinine, had a marked capacity to discriminate between patients with and without LVH; the diagnostic exclusion value (negative predictive value) is the most useful aspect, and similar results were obtained for non-normalized levels of this peptide. This fact agrees with the finding published by Ng et al2 and differs from the results obtained by Michielsen et al,9 who collected 24-hour urine in a group of patients diagnosed as having heart failure and renal dysfunction.
Finally, the urinary NT-proBNP levels, when normalized for creatinine (>37 pg/mg), were a good independent predictor of LVH. Moreover, the fact that age is also a predictive factor coincides with the high prevalence of hypertrophy in elderly subjects reported in previous studies.10
However, this study has certain limitations, such as the use of the first urine of the morning rather than that collected over 24 hours. Furthermore, the Cobas 6000 E-601 analyzer from Roche was originally designed to measure plasma NT-proBNP concentrations. Moreover, the sensitivity of the determination of NT-proBNP in urine was 55%, although the negative predictive value was good. Finally, patients with essential HT received conventional therapy that can influence the NT-proBNP levels.
In conclusion, the urinary NT-proBNP concentration can be useful for detecting LVH in patients with HT. These findings suggest the possibility of utilizing this relatively simple, noninvasive analysis under specific conditions in which the collection of plasma samples may be especially difficult or in situations in which its use is considered more appropriate, such as in the primary care setting.
Source of funding: Fondo de Investigaciones Sanitarias del Instituto Carlos III, Spain.
Correspondence: Dr. M. Rivera.
Centro de Investigación. Hospital Universitario La Fe. Avda. Campanar, 21. 46009 Valencia. España.
E-mail: rivera_jmi@gva.es
Received October 30, 2008.
Accepted for publication February 17, 2009.