Keywords
INTRODUCTION
Platypnea-orthodeoxia is a rare syndrome characterized by dyspnea (platypnea) and arterial hypoxemia in the upright posture (orthodeoxia), both conditions improving in the decubitus position. It is not associated with pulmonary hypertension. Right-left shunt occurs with no apparent cause. Interatrial communication is the cardiac abnormality more frequently associated with this syndrome. In addition, associated aortic elongation is a rather frequent finding (in fact, the 2 patients described present this). Other associated abnormalities are pneumonectomy, emphysema, or liver cirrhosis. We describe 2 clinical cases of platypnea-orthodeoxia syndrome associated with a patent foramen ovale (PFO) with right-left shunt who underwent transcatheter closure using an Amplatz device (Amplatz, AGA Medical, Golden Valley, MN, USA). After implantation, there were changes in arterial oxygen saturation and subsequent clinical improvement in the patients.
CLINICAL CASES
Case 1
Woman, 83 years old, with a background of hypertension, hypothyroidism and bilateral hypoacusis, initially admitted due to presenting 2 episodes of dysphasia and loss of strength in the left side of the body 48 h previously, with subsequent complete recovery. Progressive dyspnea of 1 month's evolution was also present improving with rest and in the decubitus position, worsening when upright.
It should be pointed out that, at admission, arterial oxygen saturation was 85% and there was grade III/VI systolic murmur with a pulmonary focus. Electrocardiogram (ECG) demonstrated a sinus rate of 80 beats/min, with a right bundle branch block pattern. Hemogram, blood biochemical analysis, thyroid hormones, and urine were normal. There were no pathological findings with cranial computed tomography (CT) or signs of acute ischemia. Chest x-ray demonstrated marked aortic elongation without cardiomegaly. Spirometry showed: FVC, 1.49 l; FEV1, 1.13 l, and a Tiffeneau index, 75.3%. Signs of carotid atheromatosis in the supraaortic arteries were found using Doppler ultrasound. Transthoracic echocardiogram (TTE) showed a dilated aortic root (39 mm) and normal pulmonary artery pressure, without other significant findings. Transesophageal echocardiogram (TEE) detected dilated aortic root (40 mm diameter), without signs of failure. Atrial septal aneurysm was present, with patent foramen ovale (PFO) and right-left micro-bubble flow (agitated physiological saline) at rest and after Valsalva maneuver. Micro-bubble flow increased in the upright position (Figures 1 and 2). Transcatheter closure of the PFO with an Amplatzer device was indicated due to the incapacitating symptoms caused by orthodeoxia.
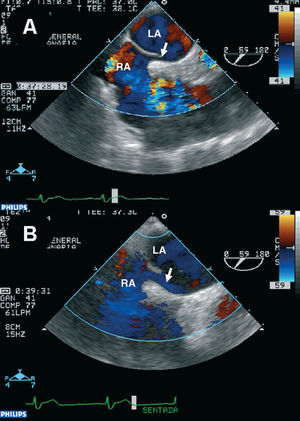
Figure 1. Transesophageal echocardiogram at the middle-third rotated through 59 degrees. Color Doppler ultrasound shows the increase in shunt and size of the abnormality (arrow) in the seated position (B) compared to that in the decubitus position (A). RA indicates right atrium; LA, left atrium.
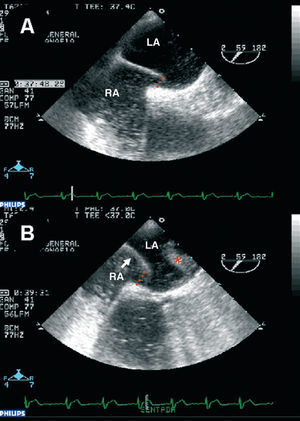
Figure 2. Transesophageal echocardiogram showing micro-bubble flow from the right atrium through the foramen; this is more evident (*) in the sitting position (B) than in the decubitus position (A). RA indicates right atrium; LA, left atrium.
Case 2
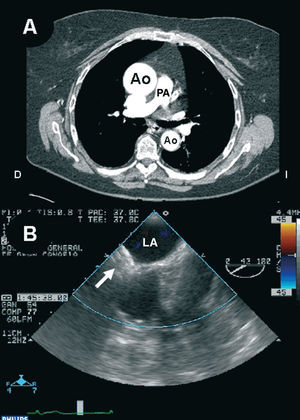
Woman, 66 years old, with a background of hypertension and stroke in the left cerebellar hemisphere without sequelae. No known coronary heart disease or bronchopathy were reported. She was admitted due to syncopal episodes followed by intense dyspnea, with partial acute respiratory failure. Physical examination showed normal cardiopulmonary auscultation; baseline tests were also normal. Hemogram and coagulation were normal, and blood biochemical tests showed a creatinine level of 1.6 mg/dL, the remaining tests proving normal. Electrocardiogram demonstrated sinus rhythm with left axis deviation. Chest x-ray demonstrated aortic elongation. Transthoracic echocardiogram demonstrated dilated aortic root (52 mm) and left ventricle hypertrophy, without pulmonary hypertension findings. Doppler ultrasound examination of the legs and pulmonary angiography were both normal. Computed tomography of the thorax showed aortic root aneurysm (Figure 3A). After the patient was transferred to the ward and began to sit, there was a greater degree of dyspnea, cyanosis and hypoxemia, leading to worse results in the arterial blood gas analysis. All these changes markedly improved upon returning the patient to the decubitus position. Transesophageal echocardiogram (with the patient in various positions) detected normal biventricular function, aortic root elongation protruding into the right atrium and marked displacement of the interatrial septum toward the left atrium when the patient was sitting. In addition, PFO was observed with right-left shunt which increased in the sitting position.
Figure 3. A: contrast material-enhanced coronal computed tomography of the great vessels where enlargement of the proximal part of the aorta can be seen. B: transesophageal echocardiogram showing the location of the Amplatzer device (arrow) in the interatrial septum. Ao indicates aorta; LA, left atrium; PA, pulmonary artery.
Symptoms caused by orthodeoxia led to transcatheter closure of the PFO with an Amplatzer device. Table 1 shows the results of arterial blood gas analysis for both patients.
Procedural Protocol
The implantation technique has been previously described in detail.1 This was carried out under angiography and ultrasound monitoring (TEE). The right atrium was accessed via the femoral vein, placing the guidewire in the left upper pulmonary vein via the PFO. The device was introduced via the catheter positioned in the left upper pulmonary vein, where the left part was released while advancing it toward the septum, finally releasing the right side leaving it placed on the interatrial partition. Correct orientation and fixation of the device were confirmed before releasing it. The entire process was done under TEE monitoring to optimally assess the most suitable place to pass the device through the septum (the septum often presents non-central fenestrations that hinder correct positioning of the device). Transesophageal echocardiogram monitoring is essential for deploying the Amplatzer device in order to correctly orientate it in relation to the septum, as well as to ensure stability once released (Figure 3B).
Vancomycin, 500 mg/6 h i.v. (4 doses), and gentamycin 80/12 h i.v. (2 doses) were administered in the ward. Subsequent evolution was satisfactory, with no complications arising from the implantation procedure. At discharge, treatment consisted of aspirin, 100 mg/day for 6 months; clopidogrel, 75 mg/day for 1 month; low-molecular-weight heparin for 10 days; and oral second-generation cephalosporin for 15 days.
DISCUSSION
Platypnea-orthodeoxia is a rare syndrome characterized by dyspnea and hypoxia in the upright position. It was described for the first time in 1949 by Burchell et al.2 Several groups of disorders have been associated with platypnea-orthodeoxia syndrome, such as some lung diseases (pulmonary arteriovenous shunt, chronic obstructive pulmonary disease, pneumonectomies, hepatopulmonary syndrome, lung embolisms, adult respiratory distress syndrome), intracardiac shunt (foramen ovale), and autonomic neuropathy or certain extrathoracic disorders (liver diseases, ascites).3-6 It is frequently associated with aortic aneurysms.7,8 Pneumonectomy seems to be the disorder most frequently associated with platypnea-orthodeoxia. It is highly probable that platypnea-orthodeoxia syndrome is more common than the number diagnosed, due to the high frequency of many of the processes associated with it.9 Thus, when intolerance to the upright position associated with hypoxia is present plus some of these other factors, transcranial Doppler ultrasound imaging and/or TEE should be done in order to rule out PFO.
One of the first attempts to explain the syndrome10 referred to distortion of the interatrial septum, which is more evident in the upright position and enables the inferior vena cava to receive shunt via the PFO (as in fetal circulation).
Surgical closure of the interatrial defect is not free from complications and involves a more than negligible morbidity and mortality rate. Currently, the percutaneous approach is the treatment of choice in patients requiring closure of the interatrial defect.11,12 Implantation is successful in a very high percentage of patients and is done in very little time under local anesthesia and ultrasonic and fluoroscopic guidance.
Some groups do not systematically use TEE during the implantation procedure.13 However, monitoring the procedure via TEE is very useful, since it makes it possible to ensure that the device used is of optimal size, rules out the presence of leaks once placed in position (allowing repositioning and/or removal in case of inadequate placement) and rules out procedural complications. There are few complications during and following implantation (embolization, infections, arrhythmias, thrombosis due to the device, persistent and extensive residual shunt, and traumatic fistulas between the aorta and left atrium which easily occurs in cases of aortic aneurysm).14
The results obtained in our 2 cases suggest that transcatheter closure of PFO is a suitable procedure for the symptomatic treatment of platypnea-orthodeoxia syndrome, particularly if it is associated with paradoxical embolism.
Correspondence: Dr. J.R. Ortega Trujillo.
Servicio de Cardiología. Hospital Universitario de Gran Canaria Dr. Negrín.
Barranco la Ballena, s/n. 35020 Las Palmas. España.
E-mail: jorttru@gobiernodecanarias.org
Received April 4, 2005.
Accepted for publication June 2, 2005.