Implantable cardioverter-defibrillators (ICD) are the standard treatment to prevent sudden death from ventricular arrhythmias.1 Traditional devices require vascular access for electrode implantation, with the consequent risk of complications such as electrode dislodgement or fracture, thrombosis, or infection.2,3 However, vascular access can prove difficult or even impossible in certain patients, such as those with certain congenital conditions that limit the use of traditional devices.
The subcutaneous ICD (S-ICD, Cameron Health, San Clemente, California, USA) avoids the need for intracardiac electrode implantation, facilitates the removal procedure, and does not require fluoroscopic guidance.
We present the clinical case of a man aged 32 years with a single-ventricle congenital heart disease, with transposition of the great arteries, atrial septal defect, and pulmonary stenosis. In 1998 he underwent a De Leval right subclavian pulmonary fistula4 and, in July 2001, complete cavopulmonary shunt and closure of the fistula.
Since 2009 he had experienced several sudden episodes of syncope. Echocardiography revealed a dilated left ventricle with very depressed systolic function (30% ejection fraction) and right ventricular hypoplasia. The aorta was dilated, with wide interventricular septal defect override and substantial pulmonary artery hypoplasia. We found no flow through the valve but did observe distal venous flow proceeding from the bidirectional cavopulmonary shunt.
In 2009 the patient underwent electrophysiologic study of the systemic ventricle by retrograde arterial access. Sustained ventricular arrhythmias were not induced nor were conduction abnormalities observed. A subcutaneous episode recorder was implanted, which later detected nonsustained ventricular tachycardias coinciding with presyncopal episodes.
Given the high risk of sudden death in this patient (class IIa indication for ICD therapy) and the fact that transvenous electrode implantation was impossible, it was decided to implant a subcutaneous ICD.
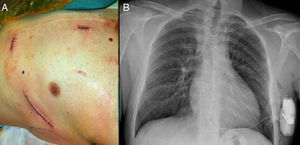
With local anesthesia and conscious sedation, an incision was made at the level of the xiphoid process and left midaxillary region (fifth left intercostal space, a location that has proved the most efficacious in previous studies4), after which we dissected by planes and constructed the pocket to deploy the generator. We then advanced the electrode until reaching the incision in the xiphoid process, and fixed it to the fascia. Next, taking the distal tip of the electrode as a reference, we made a third incision at this level, 1cm to the left of the midsternal line. We introduced the electrode and fixed the distal tip to the fascia. Finally, we connected the generator to the electrode, fixed it to the muscle plane, and then sutured by plane (Fig. 1).
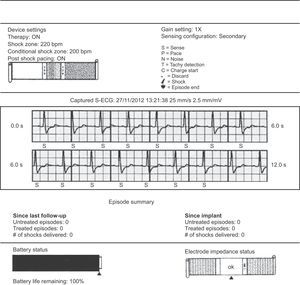
At the end of the procedure, we performed a defibrillation test. To do so, we defined a zone at 170bpm and programmed a 65 J shock. After three induction attempts with alternating current, we induced only one correctly-sensed nonsustained ventricular tachycardia. Finally, given that inducing sustained ventricular fibrillation was impossible, we opted for the conventional polarity configuration, which can revert episodes of induced ventricular fibrillation in 93% of patients,5 and administered a 10 J manual shock. We programmed a conditional therapy zone at 200bpm and the therapy zone at 220bpm (Fig. 2).
At 2 months follow-up, the patient has presented no complications and no significant events have been recorded.
The subcutaneous ICD can be the only alternative available to prevent sudden death in patients with complications derived from transvenous electrodes, venous occlusion, and anatomic abnormalities that prevent vascular access. One recent multicenter study6 shows the efficacy and safety of the subcutaneous ICD by comparison with conventional ICDs, and a current randomized multicenter study will enable us to compare both devices.
The disadvantages of the subcutaneous ICD include its slightly larger size and the fact that it does not facilitate anti-bradycardia stimulation or anti-tachycardia overstimulation therapy. At the time of writing (February 2013), the subcutaneous ICD is not yet commercially available for extensive use in Spain.