Keywords
INTRODUCTION
The prognostic value of high-sensitivity C-reactive protein (hs-CRP) has been extensively studied in ischemic heart disease.1 However, the significance of this marker in percutaneous coronary interventions (PCIs) may differ, because mechanical damage to the vessel wall can, in itself, induce a systemic inflammatory response.2 In addition, the differences between samples obtained at baseline and those taken following the procedure have not been well-established.
The aim of this study is to assess hs-CRP values in serial samples from a prospective group of patients who underwent implantation of a bare-metal coronary stent.
METHODS
From May 2002 to January 2003, 68 consecutive patients, 12 (18%) with stable angina and 56 with non-ST-elevation acute coronary syndrome (NSTEACS), were included in an open, prospective study on hs-CRP values in PCIs. All patients had received at least 1 bare-metal coronary stent. The main aim of the study was to predict major adverse coronary events (MACEs) at 1 year, defined as death, acute myocardial infarction (AMI), and the need for a new coronary revascularization procedure. Patients with transmural AMI and ST segment elevation, prior coronary revascularization, drug-eluting stents, abciximab, or eptifibatide administration (because of the anti-inflammatory action of these drugs), patients with infectious, neoplastic, or systemic diseases with associated inflammation that could be confused with the inflammatory status of ischemic heart disease, and patients who developed MACE before completion of serial sample collection. Post-PCI AMI was established on troponin T (TnT) elevation 32.5 times the normal values. All patients agreed to participate in the study. Follow-up was conducted by personal interviews or by contacting family members or physicians outside the hospital.
Bare-metal stent implantation was performed by standard techniques, generally with a radial access. The outcome was considered satisfactory when there were no immediate complications and residual stent stenosis was <20%. Following PCI, all patients received clopidogrel for at least 1 month, as well as aspirin, beta-blockers, and statins indefinitely. Any other medication was prescribed at the discretion of the attending physician.
Serial blood samples for hs-CRP analysis were taken immediately before PCI, after stent implantation, at 8 and 24 h, and at 30 days. Serum was obtained by centrifugation and stored at -20°C until analysis. Quantitative determination of hs-CRP was done by the N latex CRP mono assay with a Behring NB II nephelometer (Dade Behring, Marburg, Germany). TnT determination was performed with Troponin T STAT reagent (Roche Diagnostics).
Statistical Analysis
Categorical variables are expressed as percentage and quantitative variables as the mean (standard deviation [SD]) or median (interquartile range), depending on whether or not they followed a normal distribution. hs-CRP values at each sampling time point were compared with the Mann-Whitney U test. Categorical values were compared with Pearson's c2 test. The sensitivity and specificity of hs-CRP samples taken at the different time points was determined by receiver operating characteristic (ROC) curves, calculating the area under the curve for each time point. Using the sample that showed greatest sensitivity and specificity, a table was designed with the coordinates of the curve, and the cut-off point for hs-CRP that marked the highest sensitivity and specificity was determined. Multivariate analysis could not be performed because of the limited sample size. Event-free survival was analyzed with the Kaplan-Meier method and the curves were compared with the log-rank test. A P value less than .05 was considered significant. All analyses were performed with SPSS 14.0 (SPSS, Inc., Chicago, Illinois, USA).
RESULTS
The study included a total of 68 patients. Two patients were excluded because of TnT elevation more than 2.5-fold the normal limits (0.60 and 0.74 µg/mL) in the first 24 h. There were no exclusions between 24 h and 30 days. The clinical characteristics of the study population are summarized in Table 1. Mean age of the women was higher than that of the men (67 [9] vs 58 [10] years; P=.01). Median follow-up was 16.6 (range, 15.3-19.4) months. Patients who experienced a MACE and those that did not showed no significant differences at baseline.
The Box-Whisker chart shows that hs-CRP values always rise following PCIs, reach maximum values at 24 h, and return to normal or near-normal values at 30 days (Figure 1).
Figure 1. Box-Whisker chart showing results of serial hs-CRP determinations in PCI with bare-metal stent placement, stratified according to clinical diagnosis. AMI indicates acute myocardial infarction; PCI, percutaneous coronary intervention; hs-CRP, high-sensitivity C-reactive protein; TnT, troponin T.
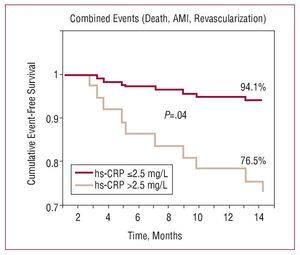
Figure 2. Estimated cumulative event-free survival (Kaplan-Meier) at 12 months, according to high-sensitivity C-reactive protein concentration (hs-CRP) >2.5 mg/L or not at 30 days following bare-metal stent implantation.
AMI indicates acute myocardial infarction
he following MACEs were recorded: 3 deaths due to cardiac causes (2 sudden deaths and 1 cardiogenic shock) and 7 percutaneous revascularizations, all for in-stent restenosis. The 3 patients who died were men and were older than the survivors (72 [5] and 60.4 [10] years; P=.06). Mean time before the development of events was 129 (107) days. High-sensitivity CRP values in patients who developed a MACE versus those who did not showed no significant differences in samples taken before the PCI, after the PCI, or at 8 h, but were more elevated at 24 h (23.30 [range, 9.90-42.00] vs 10.75 [range, 6.04-19.1]; P=.05) and at 30 days (7.15 [range, 2.54-9.20] vs 2.25 [range, 1.30-5.00]; P<.02) (Table 2). The increase at 24 h relative to baseline showed no significant differences (D=2.9 and D=2.5; P=.45).
The various ROC curves for samples taken before 24 h showed no significant differences for predicting MACEs. In contrast, the areas under the curve for 24 h (0.72 [0.55-0.89]; P=.017) and 30 days (0.77 [0.62-0.92]; P=.003) were both similarly significant for predicting events. The cut-off value that provided the highest sensitivity (80%) and specificity (72%) in the 30-day curve was 2.5 mg/L. An hs-CRP value >2.5 mg/L at 30 days was associated with a 6.15-fold increase in the risk of experiencing a MACE. Event-free survival (Kaplan-Meier) at 12 months was significantly lower when hs-CRP was >2.5 mg/L than when it was £2.5 mg/L (76.5% vs 94.1%; P=.04).
DISCUSSION
A recent study involving sample collection in the coronary sinus has shown that the mechanical compression produced by balloon inflation and stent deployment causes CRP release from the atheroma plaque.3 For this reason, the significance of CRP elevation following PCI is still controversial. In addition, it has been hypothesized that elevated baseline CRP is associated with a higher incidence of MACEs,4 but not of restenosis.5,6 In the present study, the absence of significant differences in hs-CRP levels of patients with stable angina or NSTEACS at baseline and in relation to risk factors, should be interpreted with caution, since the study population was limited. Consistent with these findings, Ridker et al7 reported that more than 30% of patients with severe unstable angina show no hs-CRP elevation, and Heeschen et al8 indicated that the risk of restenosis is independent of prior TnT values. The influence of risk factors on CRP levels has always been considered weak and for some authors, even controversial.9
The present study, in keeping with previous efforts, shows that CRP elevation at 24 h following bare-metal stent placement may indicate a greater risk of experiencing a MACE at long term.10 The main interest of the study, however, lies in the fact that at 30 days following PCI hs-CRP is sufficiently sensitive and specific to predict late MACEs. Patients with hs-CRP levels >2.5 mg/L at 30 days had a 6-fold higher risk of experiencing a MACE at 1 year, particularly stent restenosis. These findings indicate that not only the peak inflammation in the first 24-48 h, but also persistence of a maintained inflammatory state has prognostic value following implantation of a bare-metal stent. Hahn et al11 also found CRP determination at 1 month to be useful in 87 patients followed up for 3 years after PCI, and Kinjo et al12 similarly observed that when PCR concentrations remain persistently elevated at 25 days following AMI, long-term mortality is higher. Nonetheless, this data should be confirmed in studies performed with larger patient series.
The most important limitation of this study is the small population included, a fact that did not allow multivariate analysis to establish the independent character of the relationship between hs-CRP and late MACE. Another limitation is not having determined the time at which hs-CRP levels first peaked, which may have been after 24 h. This would have allowed better assessment of the increase occurring after a PCI.
In conclusion, in patients receiving a conventional stent, hs-CRP values >2.5 mg/L at 30 days following the procedure seem to be associated with a greater incidence of late MACEs, particularly in-stent restenosis.
Correspondence: Dr. J.A. Fournier.
Espinosa y Cárcel, 57, 9.o B. 41005 Sevilla. España.
E-mail: jafournier@gmail.com
Received April 10, 2007.
Accepted for publication September 17, 2007.