Keywords
INTRODUCTION
Based on the evidence provided by clinical trials, current guidelines recommend that patients who have been diagnosed with cardiovascular disease should reduce their blood pressure to <140/90 mm Hg in the case of non-diabetics, or <130/80 mm Hg in the case of diabetics. Further, it is recommended that low density lipoprotein cholesterol (LDL-C) levels should be reduced to <100 mg/dL (2.5 mmol/L).1 Unfortunately, these therapeutic goals are not always attained.2,3
The present study tries to identify the variables involved in the control of these cardiovascular risk factors in patients already diagnosed with cardiovascular disease being monitored in the primary care setting.
METHODS
Study Design
This observational study was performed within the framework of a randomized cluster clinical trial (involving heath centers) investigating the efficacy of a cardiovascular disease secondary prevention program in the primary care setting (the PREseAP study). The present study analyzes the baseline data recorded for the patients involved.
The study subjects were patients at 42 health centers distributed across eight of Spain's 17 autonomous regions. All were diagnosed with coronary heart disease (CHD), and/or cerebrovascular disease (CVD), and/or peripheral artery disease (PAD) between January 2004 and May 2005. The methodology followed in the PREseAP study has been previously described.4
Variables Analyzed
The patients' sociodemographic information, clinical background, pharmacological treatment, and analytical results were recorded. All underwent a physical examination that involved the measurement of height, body weight, the abdominal perimeter, and the systolic and diastolic blood pressure, according to a standardized protocol.
In agreement with cardiovascular disease prevention guidelines,1 blood pressure values of <140/90 mm Hg (or <130/80 mm Hg in diabetic patients) and LDL-C values of <100 mg/dL were deemed indicative of good control of these variables.
Statistical Analysis
All calculations were performed using STATA v9.0 software for the specific design of the study. The degree of blood pressure and LDL-C control was compared against patient sociodemographic and clinical characteristics, analytical results, and the treatment they received, via univariate logistic regression analysis. Multivariate logistic regression was performed to determine the degree of control of blood pressure and LDL-C (dependent variables), introducing into each analysis the variables that were significant or clinically important in univariate analysis. A P value less than .05 was considered significant.
RESULTS
The study involved 1223 patients from 42 health centers; 70.2% were men. The mean age of the patients was 66.4 (95% confidence interval [CI], 65.5-67.4 years). The cardiovascular problem prompting their inclusion in the study was CHD in 59.7% of cases, CVD in 33.9%, and PAD in 6.5% of cases.
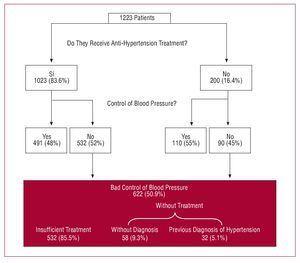
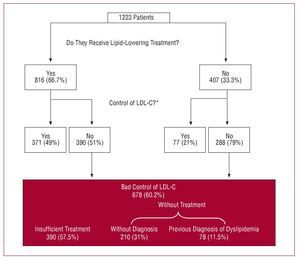
Some 83.6% (95% CI, 81-86.3) of the patients were undergoing anti-hypertension treatment and 66.7% (95% CI, 63.4-70) lipid-lowering treatment; 45.7% (95% CI, 42.3-48.9) received beta-blockers, 39.6% (95% CI, 36.6-42.6) angiotensin converting enzyme inhibitors, and 17.1% (95% CI, 14.5-19.7) angiotensin II antagonists. Some 50.9% (95% CI, 46.9-54.8) of the patients had a blood pressure of 3140/90 mmHg (or 3130/80 mmHg in diabetic patients) (Figure 1), and 60.1% (95% CI, 56.3-63.9) had an LDL-C level of 3100 mg/dL (Figure 2). Blood pressure control was deemed poor in 52% (95% CI, 47.9-56.1) of the patients treated with anti-hypertension drugs, and in 45% (95% CI, 37.6-52.3) of non-treated patients (Figure 1). LDL-C control was deemed poor in 51.2% (95% CI, 46.8-55.7) of the patients receiving lipid-lowering drugs, and in 78.9% (95% CI, 73.5-83.9) of those not treated (Figure 2).
Figure 1. Proportion of patients treated and maintained under control with anti-hypertension drugs.
Figure 2. Proportion of patients treated and maintained under control with lipid-lowering agents. LDL-C indicates low-density lipoprotein cholesterol. *Valid information from 1126 (92.1%) patients.
Tables 1 and 2 show the sociodemographic and clinical determinants associated with poor control of blood pressure and LDL-C.
DISCUSSION
This work evaluates the determinants of poor control of blood pressure and LDL-C from a clinical rather than a causal point of view (the term "determinants" is usually associated with causality, but this is not the case in the present work).
In a study of the control of high blood pressure in Spaniards over 65 years of age receiving primary care assistance,5 only 17.2% of physicians modified the treatment of patients showing poor control. In the present study, the lack of a diagnosis of heart failure was a determinant of poor blood pressure control, probably because in such patients special emphasis is placed on such control. Physician-dependent factors were not, however, investigated.
In the Hispalipid study the proportion of patients showing poor control of dyslipidemia was higher in high risk patients (84.9%) than in all patients as a whole (67.1%); it was also shown that physicians underestimated poor control.6 The EUROASPIRE II study3 showed that 58.3% of patients with coronary artery disease had total cholesterol concentrations of 35 mmol/L. In the present study, one of the determinants of poorly controlled LDL-C was the lack of lipid-lowering treatment (as might be expected); this involved a 3 times greater risk of poor control. A diagnosis of CVD or PAD increased the risk of poorly controlled LDL-C, indicating that dyslipidemia is not perceived as such an important risk factor for ictus or PAD as it is for CHD, even though statins are beneficial in the prevention of ictus and CHD.7
Few studies have examined the determinants of appropriate control of blood pressure and blood lipids in patients with cardiovascular disease. In one study it was reported that revascularized patients (monitored in outpatient clinics), obese patients, and better educated patients were those who received the best treatment and were administered lipid-lowering drugs.8 In another study that examined the control of blood pressure in patients with coronary artery disease between 6 and 18 months after hospital release, it was reported that the only predictors of poor control were age (which became poorer with increasing age) and a lack of a diagnosis of high blood pressure during hospitalization.9
The fact that not all of Spain's autonomous regions were included in the present analysis may have introduced a bias. Further, the health centers that participated in the study were possibly run by more motivated health professionals. However, the results regarding the degree of blood pressure and blood lipid control obtained were similar to those reported in other studies.3 The population with cardiovascular disease receiving care in the primary setting was therefore probably adequately represented.
CONCLUSIONS
In the improvement of the control of blood pressure in the secondary prevention of cardiovascular disease it would appear recommendable to increase the intensity of treatment (the majority of patients were already receiving some level of anti-hypertension treatment). To improve the control of LDL-C it is recommended that new lipid-lowering treatment be started (33% of patients received no such treatment), to increase the intensity of already started treatment, and to pay special attention to patients diagnosed with CVD or PAD.
PARTICIPANTS IN THE PRESEAP STUDY
Aragón: Ariño, Dolores; Abancens, Mercedes; Arroyo, Virginia; Miñana, Ana; Oliván, Bárbara; Reixa, Sol; Turón, José María.
Balearic Islands: Borrás, Isabel; Benito, Ester; Brunet, Sofía; de la Cruz, Ana Belén; Escalas, Micaela; Escriche, Luis; Fiol, Francesca; Fullana, Francisca; Fullana Inmaculada; García, Basilio; Gastalver, Elvira; Gómez, María Pía; González, María del Carmen; Hernández, María; Mattei, Isabelle; Jaume, Maria de Lluch; Llobera, Joan; Mairata, Santiago; March, Sebastià; Marimón, Margarita; Mestre, Francisca; Miguélez, Angélica; Miralles, Jeroni; Mora, Brígida; Oliver, Margarita; Ortas, Silvia; Pascual, Catalina; Pieras, Josep; Rigo, Fernando; Rodríguez, Tomás; Ruiz, Isabel María; Salas, Isabel; Sancho, Salvadora; Useros, Victoria.
Castile-Leon 1: Rodrigo, María Pilar; Bernardos, Magdalena; del Teso, José María; del Valle, María Antonia; Granja, Yolanda; Marchessi, María Jesús; Redondo, Jesús.
Castile-Leon 2: González, María Luisa; Alvárez, Violeta; De Juan, Noemí; Gonzalo, María Visitación; Higuera, Evelio; Luis, Encarna; Martínez, Itziar; Pereda, María José.
Catalonia 1: Brotons, Carlos (investigador principal); Closas, Vanesa; Corral Rosario; García, David; Gràcia, Lluís; Gutiérrez, Silvia; Iruela, Antoni; Martínez, Mireia; Moral, Irene; Morató, Maria Dolors; Palau,Antoni; Payan, Miriam; Pérez, José; Rayó, Elisabet; Soriano, Núria; Vila, Francesc; Yrla, Rosa.
Catalonia 2: Pepió, Josep Maria; Aguilar, Carina; Albero, Jordi; Arasa, Concepción; Arasa, María José; Beguer, Nuria; Bertomeu, María; Carcelle, Josep P.; Checa, Encarnación; Ciurana, Emilio; Ciurana, Maria Riera; Clua, Josep Lluís; Curto, Claudia; Dalmau, Maria Rosa; Daniel, Jordi; Fatsini, Maria Merçé; Ferré, Inmaculada; García, Gracia; Grau, Araceli; Guasch, Joan Lluís; Juan, Roland; Llor, Josep Lluís; Marín, Judit; Monclus, Josep Felip; Pons, Jaime; Ramos, Josep J.; Santigosa, Joan.
Extremadura: Buitrago, Francisco; Cañón, Lourdes; Casquero, María Pilar; Cruces, Eloísa; Díaz, Natalio; Navarro, Elisabet; Nogales, Ramón; Serrano, María Victoria; Velasco, Carmen.
Madrid: Kloppe, Pilar; Auñón, Angela; Canellas, Mercedes; Costa, Pilar; Fernández, Carmen; Garro, María Ángeles; Gómez, Rosario; Herradura, Pura; Jimeno, Milagros; Pastor, Ana; Piñero, María José; Rapp, Pilar; Segura, Roberto; Sierra, Eva.
Basque Country: Rodríguez, Ana Isabel; Benavides, Raquel; Celma, Dolores; Fuentes, Conchi; Ortueta, Pedro.
Valencia: Orozco, Domingo; Carratalá, Concha; Codorniu Miguel Ángel; Espinosa, Rosana; Fluixa, Carlos; Galán, José; Galinsoga, María del Carmen; Galofre, Manuel; Gil, Vicente; Huertas, Adela; Lluch, Francisco; López, María Isabel; Maiques,Antonio; Marco, Rocío; Martínez, Nieves; Mas, Francisco; Navarro, Jorge; Navarro, Mercedes; Payá, José Jorge; Pereira, Avelino; Prieto, Isabel; Quirce, Fernando; Richart, Miguel; Séller, María Jesús; Sevilla, Fernando; Sierra, Eva; Siurana, Milagros; Soler, José Manuel; Terol, Cecilia; Tomás, Adela
Committee adviser: Diògene, Eduard; del Río, Alfonso; Gil, Antonio; Gordillo, María Victoria; Muñoz, Miguel Ángel; Vidal, Xavier; Villar, Fernando.
A full list of the participants in the PREseAP study is provided at the end of this paper.
This project was coordinated and financed by the FIS (PI031421), Instituto de Salud Carlos III, Ministerio de Sanidad y Consumo, and received logistic support from the Investigación Cooperativa RedIAPP and RECAVA research networks. This study appears in the International Standard Randomized Controlled Trial Register ISRCTN with no 18578323.
Correspondence: Dr. C. Brotons.
Unidad de Investigación EAP Sardenya. Sardenya, 466. 08025 Barcelona. España.
E-mail: cbrotons@eapsardenya.cat
Received March 30, 2007.
Accepted for publication September 18, 2007.