Pulmonary veno-occlusive disease (PVOD) is a rare cause of pulmonary arterial hypertension. PVOD shares many characteristics with idiopathic pulmonary arterial hypertension, making it very difficult to distinguish between these conditions. Accurate diagnosis is essential because PVOD has a worse prognosis, and treatment with specific vasodilators can trigger acute pulmonary edema. Currently, the only effective treatment is lung transplantation.1
We present the case of a 74-year-old woman who was initially diagnosed with pulmonary arterial hypertension and was treated with macitentan and sildenafil. The patient showed significant improvement with this treatment, even though subsequent diagnosis revealed that she very likely had PVOD.
The patient's medical history included Sjögren syndrome, diagnosed several years previously based on presentation with dry eyes and a positive antinuclear antibody test.
The patient was first admitted in January 2015 with a diagnosis of severe congestive heart and respiratory failure secondary to atrial flutter with a rapid ventricular response. On admission, echocardiography revealed evidence of severe pulmonary hypertension and right ventricular dysfunction, whereas left cavity dimensions and function were normal (left atrium anteroposterior diameter, 33mm). Symptoms improved substantially with diuretic therapy and reversion to sinus rhythm, and the patient was discharged. She was readmitted 1 month later with similar symptoms, but this time in sinus rhythm. The decision was taken to conduct the battery of diagnostic tests recommended for the study of pulmonary hypertension: abdominal ultrasound, serology for hepatotrophic and human immunodeficiency viruses, respiratory function tests, lung computed tomography with contrast, and ventilation-perfusion scintigraphy.2,3 These tests revealed no major involvement. The study was completed with a right-side catheterization that revealed severe pulmonary arterial hypertension (pulmonary artery occlusion pressure, 7mmHg), with highly elevated pulmonary arterial resistance and severely impaired cardiac output (Table). A nitric oxide vasodilation test conducted during the same catheterization was positive according to current guidelines,2,3 and treatment was therefore commenced with calcium antagonists. The patient showed a good initial response to increasing doses of amlodipine; however, at the end of May she was readmitted with congestive heart failure.
Prognostic Variables Before and After Treatment With Macitentan and Sildenafil
| WHO-FC | No. admissions | TAPSE | S | FSRV area | RVEF (MR) | |
|---|---|---|---|---|---|---|
| Before | III | 5 | 11 mm | 7 cm/s | 25% | |
| After | II | 1 | 22 mm | 12 cm/s | 47% | 47% |
| 6MWD | CI | PVR | PAPm | RAP | BNP | |
| Before | 144 m | 1.9 L/min/m2 | 12 WU | 36 mmHg | 4 mmHg | 2791 pg/mL |
| After | 325 m | 3.28 L/min/m2 | 6.4 WU | 42 mmHg | 8 mmHg | 87 pg/mL |
BNP, brain natriuretic peptide; CI, cardiac index; FSRV area, fractional shortening of right ventricular area; PAPm, mean pulmonary arterial pressure; PVR, pulmonary vascular resistance; RA, right atrium; RAP, right atrial pressure; RVEF (MR), right ventricular ejection fraction measured by magnetic resonance; S, systolic tricuspid annular velocity measured by Doppler tissue imaging; TAPSE, tricuspid annular plane systolic excursion; WHO-FC, World Health Organization functional class; WU, Wood units; 6MWD, 6-minute walk distance.
A diagnostic review revealed that the patient had limited systemic sclerosis (calcinosis, telangiectasias, microstomia, Raynaud phenomenon, and positive tests for anti-centromere, anti-sp100, and anti-pM-scl antibodies). The worsening condition was attributed to the nonresponsiveness of patients in this subgroup, and the decision was taken to start treatment with macitentan at 10 mg/d.
The response over the following months was clearly satisfactory, albeit insufficient. In September 2015 sildenafil was added at a dose of 20mg/8h, and a few weeks later the patient was once again admitted with worsening breathlessness and congestive heart failure. A cardiac nuclear magnetic resonance examination showed no signs of left heart disease and indicated acceptable right ventricle function. Repeat right heart catheterization confirmed clear improvement in cardiac output and pulmonary artery resistance (Table). Even after administration of 500mL physiological saline solution, the pulmonary artery occlusion pressure remained below 17mmHg at all times, definitively excluding a combination of heart failure with preserved ejection fraction.
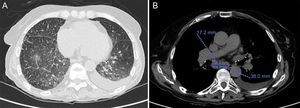
A high-resolution lung computed tomography scan was requested and demonstrated a centrilobular distribution of nodular ground-glass opacities, mediastinal lymphadenopathies of up to 3.8cm diameter, and septal thickening (Figure). In repeat tests, all respiratory functions were normal except for extremely low lung carbon monoxide diffusion capacity (DLCO) after adjustment for alveolar volume (DLCO/AV 44%) and severe chronic hypoxemia. Together, these findings very strongly suggested that the patient had PVOD associated with systemic sclerosis.
Today, more than 1 year after symptom onset, the patient is in dyspnea functional class II/IV. Her condition shows no sign of deterioration, her brain natriuretic peptide concentration is normal, her 6-minute walk distance is about 325 m, and her echocardiography-measured right-ventricular function parameters and cavity size are also within the normal range. Her situation is thus stable and satisfactory (Table) and given the risk of complications we have no plans to intensify treatment.
Diagnostic confirmation of PVOD requires histological analysis; however, lung biopsy is contraindicated in most patients. Lung computed tomography is currently considered a major diagnostic tool, and the 3 radiological signs found in our patient together give a specificity of up to 100%.2 In addition, a DLCO below 55% has a specificity of 89.5%, and the diagnosis is further strengthened by the right-side catheterization data and the respiratory failure.
The initiation of specific treatment in PVOD patients carries a recognized risk of acute pulmonary edema. Nonetheless, improvements with these therapies have been documented in small series and individual cases, the vast majority with low dose epoprostenol. To date, only minor and transient improvements have been documented with oral vasodilators,4 and there is only 1 reported positive experience with combined treatment.5 This is thus the first report of a clear improvement with combined oral therapy and a beneficial effect of macitentan in the treatment of PVOD.