Ischemic heart disease is the main cause of death in developed countries. Acute ST-segment elevation myocardial infarction (STEMI) is the most acute manifestation of coronary artery disease and is associated with high morbidity and mortality. In the last century, it was well established that early diagnosis and immediate reperfusion by primary percutaneous coronary intervention are the most effective ways to improve overall outcomes by lowering the risk of post-STEMI complications, including mechanical ones.1 Reperfusion strategies in patients with STEMI are time-dependent and should ideally be implanted within the first 2hours after the onset of symptoms.2,3
The ongoing outbreak of coronavirus disease 2019 (COVID-19) has become a global pandemic. On 31 January, 2020, Spain confirmed its first COVID-19 case and since then the number of cases has increased exponentially. Early reports noted how the COVID-19 outbreak increased the difficulty of applying the standard of care treatment for STEMI patients.4
In this disturbing scenario of the COVID-19 pandemic, we report a case of STEMI in a 65-year-old woman with a history of dyslipidemia and chronic hepatitis C virus infection without significant liver disease. The patient, an active smoker, underwent surgery for cervical cancer in 2019. The malignancy was considered inactive and controlled. Due to limitations to freedom of movement in Spain during the COVID-19 lockdown, the patient remained self-isolated at home for the past 7 days, looking after several grandchildren because school classes were also cancelled.
The patient experienced typical chest pain accompanied by vegetative symptoms but because of her responsibility for looking after her grandchildren, fear of visiting the hospital in the current situation, and awareness of the mandatory need to remain isolated at home, she did not seek medical attention until 24hours after the onset of symptoms. On arrival at the hospital, the patient reported no longer having chest pain and was hemodynamically stable. She reported a 48-hour history of intermittent low-grade fever and dry cough. The patient was tachypneic and hypoxemic with an oxygen saturation of 88% improving to 98% on 3 liters of oxygen by nasal cannula. An electrocardiogram (figure 1A) was consistent with the diagnosis of acute evolved anterior myocardial infarction. Blood pressure was 100/62mmHg, heart rate 125 bpm, and heart sounds were normal on cardiac auscultation without any heart murmur. Lung auscultation revealed bibasal rhonchi. A transthoracic echocardiogram showed the presence of extensive left ventricular wall motion abnormalities associated with severe systolic dysfunction. No mechanical complications were observed. Chest X-ray showed bilateral patchy infiltrates (figure 1B) that, together with the aforementioned symptoms of fever and dry cough, led to suspicion of the possibility of COVID-19 infection. Cobas SARS-CoV-2 test (ROCHE, Spain) was positive, confirming the viral infection in the patient.
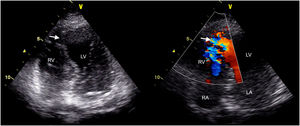
She received empirical antibiotics (ceftriaxone and azithromycin) and hydroxychloroquine as guided by hospital protocols at that time. Dual antiplatelet therapy with aspirin and ticagrelor was started. Urgent coronary angiography and percutaneous coronary intervention were not performed and were considered elective after recovery from COVID-19 infection. However, 24hours after admission, the patient showed clinical and hemodynamic instability with refractory symptomatic hypotension, oliguria, and cardiogenic shock despite vasoactive support. Physical examination revealed a new-onset holosystolic murmur and echocardiography confirmed a 13-mm apical ventricular septal defect (figure 2). As a result of the active COVID-19 infection, comorbidities, and high surgical risk in the context of a recent myocardial infarction, the patient was not considered a candidate for either surgical repair or percutaneous device closure of postmyocardial infarction ventricular septal defect. Conservative measures were adopted and the patient died the following day.
COVID-19 infection can cause pneumonia, acute respiratory distress and, eventually, death in many patients. This global pandemic could also have collateral detrimental effects on the prognosis of several diseases such as stroke, STEMI, pulmonary thromboembolism, and other time-dependent diseases. In addition, the risk of direct COVID-19-inflicted harm to the cardiovascular system, psychological stress on patients and health care providers, and infection-induced myocardial hypoxia may all contribute to the exacerbation of cardiovascular diseases.
The present case clearly illustrates how the COVID-19 pandemic can adversely affect STEMI care and its outcomes. Currently, a delay has been observed in all components of STEMI care that may further affect its associated complications and prognosis.4 On the one hand, people are reluctant to attend hospital despite warning symptoms and, on the other hand, the emergency system is markedly overloaded, leading to a delay in both the diagnosis and treatment of STEMI patients.4 Despite the lack of solid evidence, various protocols have been published by scientific societies,5,6 which aim to ensure adequate treatment of the patient with STEMI in this context, with special emphasis also on protection against infection of the health personnel involved.
CONFLICTS OF INTERESTM.Á. Arias is an associate editor of Revista Española de Cardiología; the journal has followed its established editorial procedure to guarantee impartial processing of the manuscript.