Keywords
INTRODUCTION
Pneumopericardium, defined as the presence of air in the pericardial cavity, is an uncommon but potentially very severe disease which may cause cardiac tamponade.1 Most cases have been reported in newborns receiving mechanical ventilation due to respiratory distress. The most frequent cause in adults is iatrogenic, arising as a complication of invasive procedures such as the use of mechanical ventilation or the placement of central vein catheters. Pneumopericardium has also been reported, though much less commonly, in association with other disorders such as asthma crisis, lung cancer, or esophageal perforation.2 Diagnosis is established by the presence on a chest radiograph of a paracardiac radiotransparent band in a patient with pleuropericardial-type chest pain. Computerized tomography (CT) of the chest enables a pneumopericardium to be distinguished from a pneumomediastinum because in a pneumopericardium the air changes position when the patient adopts a decubitus supine position. We report a case of pneumopericardium in a patient with community-acquired pneumonia which to the best of our knowledge is only the second case to be reported.
CLINICAL CASE
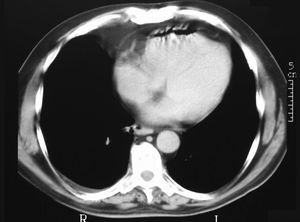
A 62-year old retired man, who had been a 2 pack/day smoker until 3 months previously, had clinical criteria of chronic bronchitis, a long history of hypertension treated with 20 mg/day enalapril, hypercholesterolemia treated with atorvastatin and an anxiety-depressive disorder treated with fluoxetine. He denied any chest trauma and had not undergone any invasive procedure. He presented to the emergency department because he noticed an acute, very intense stabbing pain in the right hemithorax when lying down. The pain had spread to the interscapular region and was accompanied by difficulty breathing deeply. He reported a three day history of general malaise, high fever and a nonproductive cough. His blood pressure was 136/80 mm Hg, the heart rate was 104 beats per minute, the respiratory rate was 28 per minute and the temperature was 39.2°C. Pulmonary auscultation revealed crepitus in the right hemithorax. Cardiac auscultation was normal with no murmurs or rubs, jugular vein swelling, pulsus paradoxus or other data of interest. The results of the laboratory tests were: leukocytes, 7.5x109/L; red cells, 2.08x1012/L; hemoglobin, 2.26 mmol/L; hematocrit, 0.42; mean corpuscular volume, 92 fl; mean corpuscular hemoglobin, 0.48 fmol/cell; platelets, 47x109/L; erythrocyte sedimentation rate, 55 mm; prothrombin activity, 50%; fibrinogen, 9.6 g/L; glucose, 6.6 mmol/L; urea, 17.4 mmol/L; creatinine, 132.6 mmol/L; total bilirubin, 70.1 mmol/L; direct bilirubin, 27.4 mmol/L; sodium, 134 mmol/L, and lactate dehydrogenase, 360 U/L. The remaining parameters, including electrolytes and liver and heart enzymes, were all normal. Baseline blood gas measurement showed a pH of 7.47, an O2 pressure of 52 mm Hg, a CO2 pressure of 28 mm Hg and an O2 saturation of 89%. An electrocardiogram showed sinus tachycardia at 110 beats per minute and an incomplete right bundle branch block, without other disorders. Chest radiography showed a consolidation with air bronchogram in the upper right lobe (Figure 1). CT of the chest to evaluate the large vessels showed the consolidation and air in the anterior pericardium, with no other findings of note (Figure 2). Transthoracic echocardiography showed slight anteroposterior pericardial separation, without hemodynamic sequelae; the rest of the study was normal. Retrospective examination of the chest radiograph revealed a small, radiolucent image parallel to the aortic button, which had not been noticed originally (Figure 1). Other studies, which were normal, included detection for Legionella antigen in the urine and a sputum Gram stain and culture with growth of a habitual saprophyte flora. Serological tests for Coxiella burnetti, Legionella pneumoniae, Chlamydia psittaci, Chlamydia pneumoniae, and Mycoplasma pneumoniae were all negative with no seroconversion after 4 weeks. The patient was treated with levofloxacin and imipenem. His course was favorable and he was discharged 10 days after admission. At a 3 month outpatient follow-up visit the patient was asymptomatic with the radiological alterations having disappeared.
Figure 1. Chest radiograph.
Figure 2. Computerized tomography of the chest.
DISCUSSION
A revision of the Medline database for the last 20 years disclosed 1 case of spontaneous pneumopericardium associated with staphylococcal pneumonia.3 The other 2 cases reported were of pneumopyopericardium, the pathogenesis of which was different from the case under discussion.4,5
We consider that the mechanism of production of the pneumopericardium in this case was due to a sudden increase in intraalveolar pressure, because other possible causes, such as trauma, the presence of fistulas from neighboring structures or infection by gas-producing pathogens can be ruled out. The increase in intraalveolar pressure due to bronchospasm or cough could provoke the rupture of some alveoli, through which the air would reach and cross the pericardiac wall, thus giving rise to the pneumopericardium.2 The small amount of pneumopericardium explains the absence of hemodynamic sequelae in this case, as well as the spontaneous resolution with no need for invasive procedures.
Although pneumopericardium is an unusual disorder, we believe it is important to bear it in mind during the differential diagnosis of chest pain in a patient with pneumonia, due to its potential seriousness.
Correspondence: Dr. J. Barquero Romero.
Avenida Alcaraz y Alenda, 20, 8.o D. 06011 Badajoz. España.
E-mail: pepebarquero@yahoo.es