Keywords
CASE STUDY
63-year-old patient, smoker of 20 cigarettes daily, with no other known cardiovascular risk factors or other clinical background of interest. The patient mentioned pleuritic pain in the left side present for 10 days before hospitalization, with a feeling of fever not confirmed with a thermometer, cough, yellowish phlegm, and worsening of clinical symptoms despite antibiotic therapy. He came to the emergency department, where the physical examination disclosed blood pressure of 130/70 mm Hg, temperature of 38°C, and heart rate of 100 bpm. The patient was eupneic, without increased jugular venous pressure, with rhythmic cardiac auscultation and no murmurs, pulmonary auscultation with decreased breath sounds in the left base and symptoms of pleural effusion, but no other alterations. The analyses showed leukocytosis with left shift, but no other relevant findings. The electrocardiogram (ECG) at admission showed sinus rhythm at 100 bpm and no other alterations. The initial chest x-ray revealed mild cardiomegaly and left pleural effusion, signs of lung hyperinflation and pulmonary hypertension. The patient was admitted to the Pneumology Department for pleural effusion study. Pulmonary perfusion scintigraphy showed that pulmonary embolism was unlikely. A second x-ray showed increased cardiomegaly and left pleural effusion with the appearance of right pleural effusion. The pleural fluid analysis revealed characteristics of an exudate, and pleural biopsy showed muscle and fibrous tissue in an insufficient specimen for diagnosis. During hospitalization, the patient had an episode of anginal chest pain associated with an episode of paroxysmal atrial fibrillation at 155 bpm that spontaneously reverted to sinus rhythm. The patient developed signs of right-sided heart failure. The echocardiogram showed mild systolic dysfunction, left ventricular ejection fraction of 51%, and mild hypertrophy. In the middle lateral wall, an extensive ventricular pseudoaneurysm was seen with rupture of the free wall of the left ventricle at this level (Figure 1). The neck of the pseudoaneurysm measured 40 mm and the aneurysmal pocket, 90x60 mm; in the interior there was blood stasis and a thrombus adhering to the wall and occupying part of the pseudoaneurysm, limited by a wall of fibrinoid appearance. Moderate to severe pericardial effusion that was causing diastolic collapse of the right atrium and ventricle was evident, and Doppler showed signs of tamponade; mild mitral regurgitation and mild dilation of the left atrium were also observed. The patient was immediately transferred to another hospital for surgery, where magnetic resonance imaging (MRI) and computed tomography (CT) (Figure 2) were performed while the operating theater was being prepared, with the patient perfectly stable and asymptomatic. The echocardiographic findings were confirmed and a second pseudoaneurysm neck and pocket was observed; rupture of the pseudoaneurysm content as well as pleural and pericardial effusion were seen. Coronary angiography showed insignificant irregularities and lesions in the right coronary artery, a severe lesion in the middle left anterior descending artery, and occlusion of the circumflex artery (Figure 3). Subsequent ventriculography showed the aneurysm and its second neck with formation of a second tubular aneurysmal pocket (Figure 3). The pseudoaneurysm ruptured during ventriculography and the patient went into cardiorespiratory arrest with transient recovery and posterior electromechanical dissociation from which he could not be resuscitated, despite transfer to the operating theater for immediate surgery.
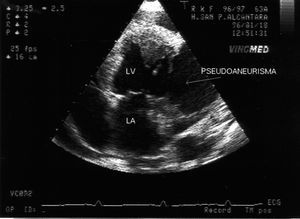
Figure 1. Four-chamber echocardiographic image showing the rupture, with tearing and thrombotic threads from the ventricular wall, the large ventricular pseudoaneurysm, and the presence of pericardial effusion.
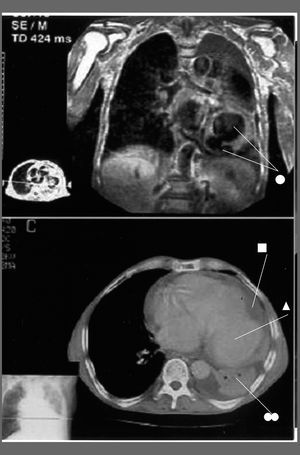
Figure 2. Magnetic resonance imaging (top) in the posterior sagittal view and scan (bottom). The arrows and square indicate the large pseudoaneurysm; the triangle and 2 circles mark the left pleural and pericardial effusion, and the single circle indicates the second aneurysmal neck evident in the MR image.
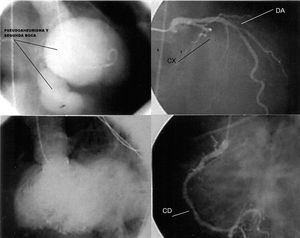
Figure 3. Coronary angiograms and ventriculography images. Circumflex (CX) occlusion, lesion in the middle left anterior descending (LAD) artery, and irregularities in the right coronary artery (RCA) can be seen, as well as the large pseudoaneurysm superimposed on the ventricular silhouette with inferior rupture and formation of a second tubular pocket in right anterior oblique (RAO) views and left anterior oblique (LAO) view.
DISCUSSION
Ventricular pseudoaneurysm is a rare entity that complicates up to 4%1,2 of all acute myocardial infarctions. It can occur in relation to chest trauma,3 heart surgery,4 or infections5,6 and is sometimes found after a silent infarction.7,8 Rupture of the free ventricular wall normally results in immediate collapse with electromechanical dissociation and death. On occasions, however, the rupture is contained by the pericardium and fibrous tissue, producing a pseudoaneurysm.
The clinical symptoms and ECG may not assist the diagnosis due to the lack of specificity.8 Unlike a true aneurysm, the wall of a left ventricular pseudoaneurysm contains only fibrous tissue and no muscle tissue. Due to the natural tendency of a pseudoaneurysm to rupture, early repair surgery is recommended, although cases of relatively good prognosis with a conservative approach have been reported.9
Our case had an abnormal presentation, with few symptoms, and no clinical or electrocardiographic evidence of prior myocardial infarction. The nonspecific discomfort, fever, and pleurocentesis results, which showed fluid with insufficiently clear exudative characteristics, did not raise clinical suspicion. The diagnosis was made on echocardiography, following an episode of paroxysmal atrial fibrillation and chest pain which indicated the need for this examination. Although the diagnosis of ventricular pseudoaneurysm is based on pathological anatomy findings, there are typical echocardiographic characteristics such as the presence of a narrow neck, thrombosis of the cavity, a fibrous wall, and flow from the ventricle to the cavity, all of them present in our patient. Other diagnostic imaging methods include conventional MRI10 or gadolinium-enhanced sequences for the wall,11 which make it possible to distinguish the presence of muscle and assist in the differential diagnosis with a true aneurysm. Helical CT12 and contrast ventriculography added to coronary angiography provide useful information. In addition to the echocardiogram (Figure 1), our patient underwent conventional MRI and CT (Figure 2), confirming the diagnosis and allowing better anatomical characterization with the presence of a second aneurysmal neck, as well as the diagnosis of complications. Coronary angiography was also performed, showing occlusion of the circumflex artery (Figure 3) and lesions in the left anterior descending artery and right coronary. As in our patient, a clinical course with minimal symptoms has been reported in other occasions.7,8 The final outcome raises some questions about the need to use aggressive diagnostic imaging methods beyond coronary angiography to provide information for surgery, when noninvasive methods are available.
Correspondence: Dr. G. Marcos Gómez.
Unidad de Cardiología. Hospital San Pedro de Alcántara.
Av. de Pablo Naranjo, s/n. 10003 Cáceres. España.
E-mail: gmarcosg@teleline.es