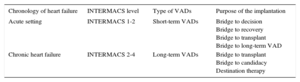
Heart failure (HF) is a major health problem that carries high mortality and morbidity.1 Approximately 5% of patients are in advanced HF and prognosis remains poor. In a small proportion of patients, heart transplant (HT) is an option. Unfortunately, the number of donors is limited, resulting in 250 HT performed per year in Spain. Consequently, mechanical circulatory support with ventricular assist devices (VADs) has emerged as a treatment option for advanced HF. The type of VAD implanted will depend on the clinical situation defined by the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) classification2 (Table). The following article aims to select the most important work published in this field in 2015.
Indications for Ventricular Assist Device Implantation
| Chronology of heart failure | INTERMACS level | Type of VADs | Purpose of the implantation |
|---|---|---|---|
| Acute setting | INTERMACS 1-2 | Short-term VADs | Bridge to decision Bridge to recovery Bridge to transplant Bridge to long-term VAD |
| Chronic heart failure | INTERMACS 2-4 | Long-term VADs | Bridge to transplant Bridge to candidacy Destination therapy |
VAD, ventricular assist device.
The annual report of the Spanish HT registry3 shows a trend toward an increased use of emergency HT (40% in recent years), with an increasing use of VADs (20%). While long-term continuous-flow VADs are the preferred option in most countries, the most frequently used in Spain are short-term VADs. Peripheral venoarterial extracorporeal membrane oxygenation (ECMO) support is the preferred option in INTERMACS 1. In patients in INTERMACS 1-2 but not in such a catastrophic situation, a short-term continuous-flow VAD is preferred, as it can provide longer support, with fewer long-term complications. However, the use of ECMO is clearly associated with worse survival and therefore, whenever possible, its use should be avoided before HT. It will be important to elucidate the reasons for this worse survival and to determine the outcomes with short- and long-term VAD as a bridge to transplant in Spain. An analysis of short-term VAD as a bridge to HT is currently underway in all HT centers in Spain and will soon provide some answers.
The INTERMACS database collects the outcome of VADs in the United States of America. Its seventh annual report1 published data on more than 15 000 long-term VADs, with a rate of 2500 patients per year in the last 2 years. The dominance of continuous flow is noticeable, with > 90% of patients receiving an intracorporeal pump, predominantly for left support. Within this group, the number of axial-flow VADs is still twice as high as that of centrifugal-flow VAD. Regarding the strategy, the increase in destination therapy (DT) is evident, with nearly 46% of implants, followed by bridge to transplant (30%) and bridge to candidacy (23%). Overall, survival at 1-year was 80%, but was worse in biventricular support (50%) and DT (76%). Several risk factors for mortality are described, such as increasing age, female sex, higher body mass index, ventilator use, INTERMACS levels 1-2, right VAD in the same operation and data suggestive of failure of other organs. The main causes of early death were right HF, neurologic events, and multisystem organ failure, while infection played an important role in late mortality.
ROADMAP4 is the first study to assess the use of long-term VADs in patients with ambulatory HF (INTERMACS 4-7). All patients met indications for VAD as DT, had ≥ 1 hospitalization in the last year, and 6-minute walk distance < 300 meters. Two hundred patients were included and assigned to medical treatment vs VAD on the basis of patient or physician choice, not randomization. Survival on original therapy with improvement in 6 minutes walking test > 75 m at 1 year, was better in the VAD group (39%) compared with medical treatment (21%), P = .012. The difference was driven by delayed VAD implant in the medical treatment group. Health-related quality of life and depression improved more significantly with mechanical circulatory support. However, a composite of adverse events that included bleeding, infection, thrombus, stroke, arrhythmias, and worsening HF was twice as common in the VAD group (1.89 events/patient-year). Although the authors conclude that this study supports the use of VAD in INTERMACS 4-7, the high incidence of adverse events and the costs of VAD indicate the need for caution regarding too early VAD placement.
Stroke and bleeding still remain major adverse events and the TRACE study5 is interesting because it analyzed 100 HeartMate II patients with reduced antithrombotic therapy, which included warfarin only (38%), aspirin only (28%), or no antithrombotic agent (34%). While the rate of device thrombosis (0.08 patients-per-year) was higher than in clinical trials, subsequent bleeding occurred in 52%, despite reduced antithrombotic therapy. Therefore, although reduced antithrombotic therapy may be necessary when bleeding occurs, it should not be the standard strategy for all patients.
Finally, we must mention the first report on the initial experience with a new magnetically levitated continuous-flow VAD (Heartmate 3), which shows similar short-term results to the existing VAD technology.6 Further studies, such as the MOMENTUM 3 (NCT02224755), will compare outcomes with this new technology with those of the most commonly used axial-flow VAD.
In conclusion, VADs save lives and their use as a bridge to transplant or candidacy is unquestionable. However, their costs and rate of adverse events limit their potential as DT. The use of VADs in Spain is increasing and the management of these patients with advanced HF remains a challenge.
CONFLICTS OF INTERESTNone declared.