Hospital length of stay for ST-segment elevation acute coronary syndrome (STEACS) has traditionally been determined by the need to monitor electrical and mechanical complications during the infarction and after revascularization. However, with the increasing standardization of primary angioplasty as the treatment of choice and the establishment of emergency treatment networks, survival has increased significantly, and this has been accompanied by a reduction in the complications associated with these events.1,2 The current clinical practice guidelines of the European Society of Cardiology recommend assessment for discharge in the first 48-72hours for low-risk patients who are able to start cardiac rehabilitation early with access to suitable follow-up.3 While there are data supporting early discharge for this patient subgroup,4 to date no study has evaluated strategies for discharge of STEACS patients within 48hours. Given the negligible rate of mechanical complications in low-risk patients,1 we sought to determine the safety of discharge after a hospital stay shorter than 48hours (a maximum of 2 nights) and secondarily to assess whether this policy would bring significant cost savings.
We prospectively selected all consecutive patients admitted between January 2017 and October 2018 for ST-segment elevation acute myocardial infarction who were assessed as being at low risk. The criteria used to define low risk are listed in Table 1. The principal study aim was to assess the 30-day occurrence of any severe adverse event indicating that the patient might have been managed more appropriately under a more cautious discharge policy. The severe adverse advents considered were myocardial reinfarction, stent thrombosis, major bleeding, rehospitalization for any cause, stroke, and death from any cause. During predischarge consultation, all patients were instructed by the attending physician about the nature of their disease and received precise guidance about health care, medication, and the follow-up schedule.
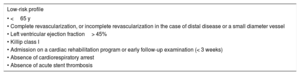
Inclusion Criteria
| Low-risk profile |
|---|
| • <65 y |
| • Complete revascularization, or incomplete revascularization in the case of distal disease or a small diameter vessel |
| • Left ventricular ejection fraction> 45% |
| • Killip class I |
| • Admission on a cardiac rehabilitation program or early follow-up examination (< 3 weeks) |
| • Absence of cardiorespiratory arrest |
| • Absence of acute stent thrombosis |
Hospitalization costs were estimated from the Community of Madrid price list for public services and activities (Orden 727/2017). This document provides cost estimates for a primary angioplasty procedure and daily hospitalization for acute coronary syndrome in a coronary unit. We used the daily cost to obtain the hourly cost. The outcome measure was the per-patient cost reduction, calculated from the difference in hospitalization hours relative to a standard hospital stay of 72hours.
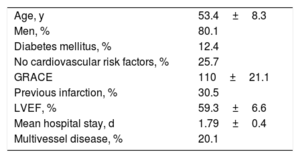
The study included 105 patients, representing 20% of the total number of STEACS patients admitted during the study period. Baseline patient characteristics are summarized in Table 2. The mean age of the study population was 53.4±8.3 years, and 19.1% (n=20) were women. Analysis of cardiovascular risk revealed that 13 patients (12.4%) had diabetes and that 25.7% had no identified cardiovascular risk factor at the time of the event.
Patient Characteristics
| Age, y | 53.4±8.3 |
| Men, % | 80.1 |
| Diabetes mellitus, % | 12.4 |
| No cardiovascular risk factors, % | 25.7 |
| GRACE | 110±21.1 |
| Previous infarction, % | 30.5 |
| LVEF, % | 59.3±6.6 |
| Mean hospital stay, d | 1.79±0.4 |
| Multivessel disease, % | 20.1 |
GRACE, Global Registry of Acute Coronary Events score; LVEF, left ventricular ejection fraction.
Unless indicated otherwise, data are expressed as mean±standard deviation.
The mean GRACE score on admission was 110.2±21.1 points, and 30.5% of infarctions were anterior. Regarding coronary anatomy, 80.9% of patients had single-vessel disease, and the rest had 2-vessel disease; there were no incidences of 3-vessel disease. Mean left ventricular ejection fraction was 59.3%±6.6%.
At the time of discharge, 62.9% of the study patients were receiving treatment with prasugrel and 32.4% were receiving ticagrelor. All patients (100%) were on statin therapy, while 70.1% were taking angiotensin-converting enzyme inhibitors and 85.1% were taking beta-blockers. The mean hospital length of stay was 1.79±0.4 days. Most of the patients (79.1%; n=83) attended the cardiac rehabilitation program at our center for a mean period of 20.1±15.9 days. The remaining 20.9% (n=22) attended a cardiac rehabilitation program or received follow-up assessment from the cardiology service at their referral center; of this group, 90.9% (n=20) attended the first follow-up visit within 3 weeks after discharge.
No events were recorded in the 30-day postdischarge period to indicate that delayed discharge would have been preferable. For the secondary aim, the reduction in hospital stay produced an estimated total saving of €206 741.60±€6069.20 (95% confidence interval, €194 713.80 to €218 769.30), corresponding to a per-patient saving of €1968.00.
This study is the first to thoroughly investigate hospital discharge of STEACS patients in under 48h. In our cohort, complications after early discharge were no worse than predicted for longer hospital stays, and there was no indication that patients would have received better treatment had they remained in hospital for longer. Moreover, while the savings were modest compared with the cost of many health care procedures, they were nonetheless substantial.
The encouraging data presented here suggest that a policy of discharging STEACS patients in under 48hours may be feasible. The results are nonetheless limited by the small sample size, and this strategy will require validation in further studies with larger numbers of patients.