Intra-aortic balloon counterpulsation (IABC) was first used in 1968. In hemodynamic terms, use of IABC is based on increasing diastolic coronary flow and systemic systolic flow, reducing afterload and myocardial work.1 Given these physiologic effects, its use extended to myocardial infarction in cases of cardiogenic shock, in the belief it would improve organ and myocardial recovery.2
European and North-American cardiology societies’ clinical practice guidelines on management of ST-segment elevation acute myocardial infarction (STEMI) strongly recommend its use (class I).3,4 Nonetheless, the rate of IABC use in patients with STEMI in Killip class IV is relatively low (20%-40%).1
The recently published IABP-SHOCK II study results concluded that IABC use does not significantly reduce mortality in patients with STEMI complicated by cardiogenic shock and undergoing early percutaneous revascularization.5 These results constitute a contradiction of current international cardiology society recommendations. The purpose of the present short study is to analyze the results of IABC use in patients with cardiogenic shock secondary to STEMI in a tertiary-care hospital.
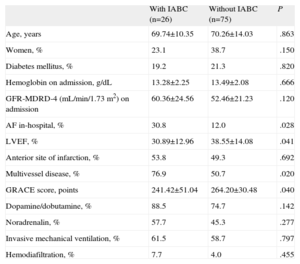
We enrolled all patients with STEMI admitted to the coronary unit of our hospital (n=1478) from 2004 through 2010 and selected those with cardiogenic shock (n=120 [8.1%]). A patient was considered to be in cardiogenic shock when systolic blood pressure was <90 mmHg for >30 min and an amine infusion was needed to hold systolic blood pressure above this value, together with signs of poor peripheral perfusion and/or pulmonary congestion. We excluded patients who did not undergo percutaneous coronary revascularization or in whom the intervention took place following >24h delay (n=19). Hence, the final sample consisted of 101 patients undergoing early percutaneous coronary intervention; IABC was used in 26 (25.7%). Table 1 shows patient characteristics. Note that a priori in-hospital risk calculated with the GRACE score was higher in patients without IABC; they also had worse renal function. However, cardiac disease, in terms of the percentage of multivessel disease and reduced left ventricular ejection fraction, was significantly greater in patients with IABC. Use of the different types of amine was similar in both groups.
Comparison of Patient Clinical Characteristics With and Without Intra-aortic Balloon Counterpulsation
| With IABC (n=26) | Without IABC (n=75) | P | |
| Age, years | 69.74±10.35 | 70.26±14.03 | .863 |
| Women, % | 23.1 | 38.7 | .150 |
| Diabetes mellitus, % | 19.2 | 21.3 | .820 |
| Hemoglobin on admission, g/dL | 13.28±2.25 | 13.49±2.08 | .666 |
| GFR-MDRD-4 (mL/min/1.73 m2) on admission | 60.36±24.56 | 52.46±21.23 | .120 |
| AF in-hospital, % | 30.8 | 12.0 | .028 |
| LVEF, % | 30.89±12.96 | 38.55±14.08 | .041 |
| Anterior site of infarction, % | 53.8 | 49.3 | .692 |
| Multivessel disease, % | 76.9 | 50.7 | .020 |
| GRACE score, points | 241.42±51.04 | 264.20±30.48 | .040 |
| Dopamine/dobutamine, % | 88.5 | 74.7 | .142 |
| Noradrenalin, % | 57.7 | 45.3 | .277 |
| Invasive mechanical ventilation, % | 61.5 | 58.7 | .797 |
| Hemodiafiltration, % | 7.7 | 4.0 | .455 |
AF, atrial fibrillation; GFR-MDRD-4, glomerular filtration rate calculated with the MDRD 4 equation; IABC, intra-aortic balloon counterpulsation; LVEF, left ventricular ejection fraction.
Data are expressed as no. (%) or mean±standard deviation.
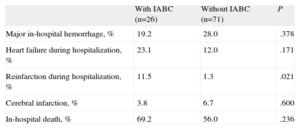
Of 101 patients, 60 died in-hospital (59.4%), with no significant differences between patients with IABC (69.2%) and without IABC (56.0%) (P=.236). Nor were there differences between the groups in the appearance of heart failure. However, the reinfarction rate was greater among patients with IABC (Table 2). Given that patients with IABC had a higher percentage of multivessel disease, we analyzed patients with single vessel disease independently. Our findings were similar to those for all patients; the death rate (66.7% vs 59.5%; P=.738) and rate of heart failure (16.7% vs 13.5%; P=.836) were similar, and the percentage of reinfarctions remained higher in patients with IABC (16.7% vs 0; P=.012). This surprising result could be explained by the higher percentage of multivessel disease in the IABC group (76.9% vs 50.7%; P=.020).
Comparison of Clinical Events in Patients With and Without Intra-aortic Balloon Counterpulsation
| With IABC (n=26) | Without IABC (n=71) | P | |
| Major in-hospital hemorrhage, % | 19.2 | 28.0 | .378 |
| Heart failure during hospitalization, % | 23.1 | 12.0 | .171 |
| Reinfarction during hospitalization, % | 11.5 | 1.3 | .021 |
| Cerebral infarction, % | 3.8 | 6.7 | .600 |
| In-hospital death, % | 69.2 | 56.0 | .236 |
IABC, intra-aortic balloon counterpulsation.
Current scientific evidence does not support widespread use of IABC in patients with cardiogenic shock. In a 2009 meta-analysis, the published data showed no benefit from IABC for patients with STEMI complicated by cardiogenic shock.6 In subgroup analysis, the authors found patients receiving thrombolysis did show benefits but those undergoing percutaneous revascularization did not. Our results, from a single-center registry of patients undergoing percutaneous revascularization, coincide with those of the aforementioned study. Recently published IABP-SHOCK II trial data will lead to a change in current clinical practice guidelines’ recommendations.5 This clinical trial involving patients with STEMI with cardiogenic shock and undergoing revascularization found no benefit from IABC use on reducing mortality versus conventional treatment. Furthermore, as secondary objectives, they analyzed length of stay in the coronary unit, dosage and duration of catecholamines, renal function, and lactate concentrations, none of which showed significant differences between groups. Rates of hemorrhage or cerebral infarction showed no significant differences either.
Therefore, to conclude, IABC use should not be generalized in patients with STEMI complicated by cardiogenic shock undergoing percutaneous coronary intervention. More studies are needed to clarify when IABC can be of use, as well as to identify the benefits of ventricular assist devices in reducing mortality and events in this patient group.