Atrial fibrillation (AF) is the most common cardiac arrhythmia and the reason for many emergency department (ED) visits.1 The treatment of AF in the ED is a challenge the recommended approach is conversion to sinus rhythm (SR).2 Rhythm control is normally achieved with propafenone and flecainide in patients without structural heart disease and with amiodarone in those with structural heart disease. Nevertheless, given the difficulty of ruling out a history of structural heart disease, intravenous amiodarone is frequently used in the ED, although it is not considered the best choice for conversion to SR. Vernakalant is a new antiarrhythmic multichannel blocking agent intended for intravenous administration with a short half-life (2 hours) and high selectivity for atrial cardiomyocytes. It is recommended for conversion in patients with AF of less than 7 days duration, moderate structural heart disease, and the only contraindications are severe hypotension (< 100 mmHg), heart failure (New York Heart Association functional class III-IV), severe aortic stenosis, or acute coronary syndrome within 30 days.2,3 Given the benefits of the drug, we began to use it in the our ED according to the recommendations on dosage and infusion times and the summary of the product characteristics.4 We present our experience of the first 52 consecutive administrations of vernakalant between January 2014 and December 2015. We collected information on risk factors, the presence of structural heart disease, duration of AF, time from start of infusion to conversion to SR, adverse effects, and length of stay in the ED.
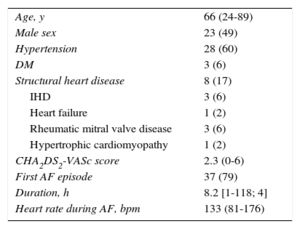
In total, 47 patients were included in the study. Of these patients, 5 received vernakalant during 2 ED visits, making a total of 52 treatments. Table 1 shows the patients’ baseline characteristics. Conversion was achieved in 45 patients (86%) and a second vernakalant infusion was needed in only 8 patients. In addition, the time to conversion to SR was rapid (mean, 12.5minutes; range, 1-115; median, 8), which led to shorter stays in the ED (mean, 5.3 [2-18] hours). Five patients experienced mild adverse events: 1 patient had sustained ventricular tachycardia (vernakalant infusion was maintained with subsequent conversion to SR); 2 patients had self-limiting cough and nausea; 1 patient had dysgeusia; and 1 patient had self-limiting atrial flutter. Regarding its use with other antiarrhythmic agents, conversion was attempted with amiodarone in 1 patient, without success, and at 4hours an infusion of vernakalant achieved conversion within a few minutes. Another patient received background therapy with flecainide to which vernakalant was added without incident. Vernakalant was used more frequently with beta-blockers (10 patients) than with dihydropyridine calcium antagonists (1 patient).
Baseline Characteristics of the 47 Patients
| Age, y | 66 (24-89) |
| Male sex | 23 (49) |
| Hypertension | 28 (60) |
| DM | 3 (6) |
| Structural heart disease | 8 (17) |
| IHD | 3 (6) |
| Heart failure | 1 (2) |
| Rheumatic mitral valve disease | 3 (6) |
| Hypertrophic cardiomyopathy | 1 (2) |
| CHA2DS2-VASc score | 2.3 (0-6) |
| First AF episode | 37 (79) |
| Duration, h | 8.2 [1-118; 4] |
| Heart rate during AF, bpm | 133 (81-176) |
AF, atrial fibrillation; DM, diabetes mellitus; IHD, ischemic heart disease.
Data are expressed as no. (%) or mean [range; median].
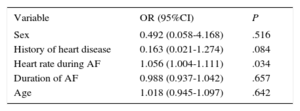
Binary logistic regression analysis was used identify predictors of success in conversion to SR with vernakalant (Table 2). Elevated heart rate on the first electrocardiogram at arrival was independently associated with successful conversion, whereas the presence of structural heart disease was associated with low success rates.
Independent Predictors of Conversion to Sinus Rhythm Using Vernakalant (Binary Logistic Regression)
| Variable | OR (95%CI) | P |
|---|---|---|
| Sex | 0.492 (0.058-4.168) | .516 |
| History of heart disease | 0.163 (0.021-1.274) | .084 |
| Heart rate during AF | 1.056 (1.004-1.111) | .034 |
| Duration of AF | 0.988 (0.937-1.042) | .657 |
| Age | 1.018 (0.945-1.097) | .642 |
95%CI, 95% confidence interval; AF, atrial fibrillation; OR, odds ratio.
This study demonstrates the efficacy of vernakalant in achieving rapid and safe conversion to SR. Only 5 patients experienced mild transient adverse effects and the mean conversion time was 12.5minutes, which allowed patients to be discharged from the ED in just over 5hours.
The results of our series are better than those of pivotal trials of vernakalant, which together show an efficacy of 51%3 although, as in our series, conversion was rapid and safe. Nevertheless, the results of its use in clinical practice are very similar to ours. Demonstrated efficacy rates of 86% to 93% and of 66% have been published by Conde et al3 and Mochalina et al5, respectively. The analysis of predictors of success showed that elevated heart rate was associated with the highest success rates. However, in line with the findings of Costabel al,6 the presence of structural heart disease was nonsignificantly associated with low success rates. This finding may explain why the results of registries are better than those of pivotal trials, given that the proportion of patients with structural heart disease is lower in real-world registries.
The main limitations of this study are its single-center design and its small sample size, which may have decreased its statistical power to identify predictors of successful conversion. In addition, the patients were relatively healthy, had a low prevalence of structural heart disease, and had a first AF episode. In contrast, the percentage of patients with a first AF episode was lower in clinical trials and other published real-world studies.
In conclusion, vernakalant is an efficacious, rapidly acting, and safe drug for conversion of AF to SR. The main limitations to its generalized use are its price and the usual concerns regarding the introduction of a new antiarrhythmic for use in the ED.
CONFLICTS OF INTERESTJ Cosin-Sales has received fees from Cardiome for presenting papers.