Because of concern about the risks posed to the fetus by ionizing radiation exposure during pregnancy, some female cardiologists rule out training as interventional cardiologists. For those already working in this area, pregnancy involves a 1-year interruption (pregnancy and maternity leave) to their careers in interventional cardiology, leading them to delay the decision to become pregnant. This letter describes the spontaneous risk of malformation/cancer in offspring, the increased risk due to radiation exposure, and the recommended dose limits for pregnant employees exposed to ionizing radiation. Little information is available in the literature on pregnant employees exposed to ionizing radiation. Here we present data from 5 interventional cardiologists in Spain who continued to work in catheterization laboratories throughout their pregnancies.
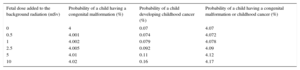
Fetal radiation exposure can lead to 2 types of adverse effects: deterministic (nonprobabilistic) and stochastic (probabilistic). Deterministic effects occur after a threshold dose and include intrauterine growth restriction, miscarriage, mental retardation, low intelligence quotient, and congenital malformations. There is no threshold dose for stochastic effects, although the probability of their occurrence rises as the dose exposure increases. The most significant is childhood cancer.1 The spontaneous probability of a newborn having a congenital malformation or childhood cancer is 4.07% (Table 1).1 It is estimated that exposure to 1 mSv during pregnancy would increase this risk by 0.008%, representing a risk of 4.078%, and that exposures of > 10 mSv would increase the risk by 0.1%.1 Experimental animal studies have shown that doses of < 100 mSv will have no effect on the embryo/fetus2 in either the preimplantation stage or organogenesis, or the fetal period. However, the question arises of what are the dose levels in interventional cardiology? What dose would be received by the fetus of a pregnant woman working in a catheterization laboratory? It is difficult to find information in the literature, although the doses appear to be extremely low. The Mayo Clinic (Rochester, United States) determined the radiation received by 68 employees (of any profession) who wore an abdominal dosimeter during pregnancy. Of these employees, 56 (82.4%), including 2 interventional cardiologists, had undetectable radiation levels in the abdominal dosimeter under the lead apron.1 To put these radiation levels into context, it is worth noting that background or cosmic radiation represents an average dose of 0.75 to 1 mSv during pregnancy and, more importantly, there are no differences in the incidence of congenital malformations/miscarriages between pregnant women exposed to doses of ≤ 50 mSv and those exposed to background radiation (< 1 mSv). The fetal doses that have been related to the occurrence of malformations/childhood cancer are > 100 to 150 mSv.1,2 These doses are much higher than those that received by an interventional cardiologist would receive under the apron. As such, if standard protective measures are used, the risk to the fetus would be negligible.
Probability of a Child Suffering From a Congenital Malformation or Childhood Cancer
| Fetal dose added to the background radiation (mSv) | Probability of a child having a congenital malformation (%) | Probability of a child developing childhood cancer (%) | Probability of a child having a congenital malformation or childhood cancer (%) |
|---|---|---|---|
| 0 | 4 | 0.07 | 4.07 |
| 0.5 | 4.001 | 0.074 | 4.072 |
| 1 | 4.002 | 0.079 | 4.078 |
| 2.5 | 4.005 | 0.092 | 4.09 |
| 5 | 4.01 | 0.11 | 4.12 |
| 10 | 4.02 | 0.16 | 4.17 |
Nevertheless, to guarantee the fetus a similar level of protection to the rest of the population, national and international radiology protection bodies recommend maximum radiation levels during pregnancy that are much lower than those demonstrated to pose a risk to the fetus. To this end, the EURATOM (European Atomic Energy Community treaty) directive sets out a maximum limit of < 1 mSv for the fetus from the time the pregnancy is reported until the birth (2 mSv in dosimeter due to attenuation of abdominal organs).3 In the United States, a limit of ≤ 0.5 mSv/mo has been established, with a total dose during pregnancy of < 5 mSv1.
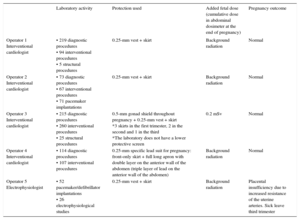
Is it possible to work in a catheterization laboratory during pregnancy? It is possible, if radiation levels are monitored using an abdominal dosimeter under the apron and suitable protective measures are used. Nowadays, instantaneous electronic dosimeters are available that offer immediate information and allow corrective measures to be taken. The use of a lead apron in the form of a 0.25-mm vest + skirt during pregnancy appears to be sufficient. The overlapping of the 2 layers of the skirt on the anterior wall of the abdomen provides protection that is equivalent to a 0.5-mm apron, and attenuates 98% of the scattered radiation (the main radiation source in interventional cardiology) (Figure 1 of the supplementary material). As the abdomen grows, the apron must be replaced by a larger one, to ensure the double layer on the anterior wall of the abdomen. Adding additional 0.5-mm skirts or aprons would minimally reduce the radiation and could lead to musculoskeletal problems. There are specific aprons for pregnant women that add a front skirt to the 2 layers of the full apron to further increase protection. The use of a 0.5-mm gonad shield attached to the inside of the lead skirt is another lighter alternative in the first trimester (Figure 2 and Figure 3 of the supplementary material). Protective screens, hung from the table or the ceiling, are an essential protective tool during pregnancy, as they attenuate 99% of the scattered radiation and reduce total radiation exposure by 50% to 75% (Figure 4 of the supplementary material). Finally, Table 2 shows the data from 4 interventional cardiologists and 1 electrophysiologist who continued to work in the laboratory during pregnancy between 2008 and 2016. In view of these data, and after reviewing the radiation levels that pose a risk to the fetus, we consider that, with suitable protection, the added risk for the fetus due to ionizing radiation exposure resulting from continuing activity in the laboratory during pregnancy is virtually negligible and is acceptable, especially if the equivalent dose received is ≤ 1 mSv. It is therefore possible for pregnant women to continue to work in the laboratory if they wish to do so.
Interventional Cardiologists and Electrophysiologist With Laboratory Activity During Pregnancy
| Laboratory activity | Protection used | Added fetal dose (cumulative dose in abdominal dosimeter at the end of pregnancy) | Pregnancy outcome | |
|---|---|---|---|---|
| Operator 1 Interventional cardiologist | • 219 diagnostic procedures • 94 interventional procedures • 5 structural procedures | 0.25-mm vest + skirt | Background radiation | Normal |
| Operator 2 Interventional cardiologist | • 73 diagnostic procedures • 67 interventional procedures • 71 pacemaker implantations | 0.25-mm vest + skirt | Background radiation | Normal |
| Operator 3 Interventional cardiologist | • 215 diagnostic procedures • 260 interventional procedures • 25 structural procedures | 0.5-mm gonad shield throughout pregnancy + 0.25-mm vest + skirt *3 skirts in the first trimester, 2 in the second and 1 in the third *The laboratory does not have a lower protective screen | 0.2 mSv | Normal |
| Operator 4 Interventional cardiologist | • 114 diagnostic procedures • 107 interventional procedures | 0.25-mm specific lead suit for pregnancy: front-only skirt + full long apron with double layer on the anterior wall of the abdomen (triple layer of lead on the anterior wall of the abdomen) | Background radiation | Normal |
| Operator 5 Electrophysiologist | • 52 pacemaker/defibrillator implantations • 26 electrophysiological studies | 0.25-mm vest + skirt | Background radiation | Placental insufficiency due to increased resistance of the uterine arteries. Sick leave third trimester |
To Marta, Leire, Teresa and Elena, for allowing me to use their personal information, and to Fina Mauri, who gave me the opportunity to discuss my own experience in the 2016 EuroPCR course.