Pseudopheochromocytoma is characterized by severe symptomatic paroxysmal hypertension (HT) similar to the clinical picture of pheochromocytoma but with normal catecholamine concentrations and the absence of an adrenal tumor on imaging study. Pseudopheochromocytoma is an infrequent entity of unknown etiology, antihypertensive treatment is generally ineffective, and many patients incur chronic disability. Although the physiopathology of this entity is also unknown, the autonomic nervous system is thought to play a fundamental role since the presence of sympathoadrenal hyperactivity has been proven.1 To treat resistant HT, an invasive technique has recently been developed, which involves percutaneous radiofrequency ablation of the sympathetic nervous system via a catheter deployed at the level of the renal arteries.2
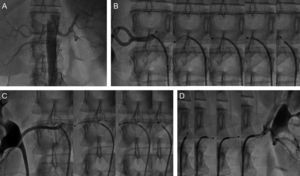
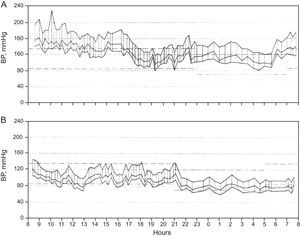
We describe the case of a 32-year-old woman with an unremarkable past medical history and longstanding hypertensive crises with values of 230/120mmHg accompanied by sweating, headache, trembling and tachycardia and lasting from 10min to several hours. Between crises, her blood pressure (BP) remained high. Other causes of secondary HT were excluded, as was pheochromocytoma, after several catecholamine determinations and diverse imaging studies.3 The final diagnosis of exclusion was pseudopheochromocytoma, and treatment was initiated with alpha- and beta-blockers, as well as psychotherapy. At the last medical visit, after an 8-year history of HT, the patient had mild left ventricular hypertrophy, with a left ventricular mass index of 116g/m2. The HT crises became less frequent, but did not disappear; HT figures remained high despite treatment with 5 drugs, including a diuretic. Percutaneous renal denervation was indicated and performed using right femoral artery access with deep sedation and a Symplicity radiofrequency catheter (Medtronic). Two 2-min radiofrequency applications were made at the level of the left, right and right accessory renal arteries (Fig. 1). The procedure was uneventful and the patient was discharged at 24h. Fifteen days before the procedure, 24-h ambulatory blood pressure monitoring recorded a mean systolic BP of 156mmHg and a mean diastolic BP of 112mmHg (Fig. 2A). At 4 weeks after the procedure, the patient—following the same drug regimen—underwent ambulatory blood pressure monitoring again, with a mean systolic BP of 111mmHg and a mean diastolic BP of 80mmHg (Fig. 2B). At 5 months, there had been no recurrence of symptomatic HT and BP values were within the normal range; the patient's drug regimen included only 1 antihypertensive agent.
A: aortogram showing a principal left renal artery and a right renal artery with an accessory artery. B: 4 circumferential radiofrequency applications, 5mm apart, at the level of the right renal artery. C: 3 applications in the right renal accessory artery. D: 3 applications at the level of the left renal accessory artery.
24-h ambulatory blood pressure monitoring. A: baseline (daytime mSBP, 163mmHg; night-time mSBP, 140mmHg; average mSBP, 156mmHg; daytime mDBP, 117mmHg; night-time mDBP, 100mmHg; average mDBP, 112mmHg; B: at 1 month post-renal ablation (daytime mSBP, 116mmHg; night-time mSBP, 100mmHg; average mSBP, 111mmHg; daytime mDBP, 85mmHg; night-time mDBP, 71mmHg; average mDBP, 80mmHg). BP, blood pressure; mDBP, mean diastolic blood pressure; mSBP, mean systolic blood pressure.
The physiopathology of pseudopheochromocytoma is currently unknown, although the principle mechanism is thought to be activation of the sympathetic nervous system (increased dopamine and epinephrine secretion and some hypersensitivity of the adrenergic receptors), often associated with an emotional factor.1 Given how little is known, treatment is usually complex and includes 3 approaches: antihypertensive treatment (a regimen of alpha- and beta-blockers is usually recommended); psychopharmacologic treatment (antidepressants and benzodiazepines), and psychotherapy, although in 40% of patients or more it is ineffective.4 Sympathetic nervous system ablation may be a therapeutic option in the subgroup of patients with resistant HT and paroxysmal crises associated with proven sympathetic hyperactivity. To our knowledge, this is the first description of a case of pseudopheochromocytoma efficiently treated by percutaneous ablation of the sympathetic renal arteries. We consider it likely that patients with this condition may have been enrolled in the Symplicity HTN (Renal Denervation in Patients With Uncontrolled Hypertension) studies. Although we cannot totally exclude a placebo effect for the intervention in this patient, preprocedural ambulatory blood pressure monitoring during refreshing sleep showed high BP levels that clearly improved postprocedure, reducing the likelihood of a placebo effect. The randomized Symplicity HTN-2 study demonstrated that renal denervation was a means of controlling BP in patients with resistant HT but 10% to 20% of patients did not respond.2 In future, we will have to identify the subgroup of patients who, a priori, have a high probability of responding. These patients with resistant HT and paroxysmal crises secondary to adrenergic hyperactivity seem ideal candidates for this technique. The Symplicity HTN studies excluded patients with accessory renal arteries; the spectacular response of our patient could also be related to accessory artery ablation, although this is pure speculation. Notwithstanding, the effectiveness of percutaneous renal denervation needs corroboration through a longer follow-up.
.