Coronary physiological indices are not widely used, despite evidence supporting their utilization.1 This is largely because of confidence in the adequacy of angiographic assessment and because measurement of these indices requires coronary guidewire manipulation2 or, in the case of fractional flow reserve (FFR), induction of hyperemia.3
A number of simplified indices have been developed to increase the use of functional assessment. These include instantaneous wave-free ratio [iFR], diastolic resting pressure ratio [dPR], resting full-cycle ratio [RFR], and quantitative flow ratio (QFR).4 The success of iFR spawned the development of other indices not requiring hyperemia induction, such as RFR, which has been shown to have good correlation and agreement with iFR and FFR in retrospective analyses.5 In addition, QFR does not require the use of a guidewires as it is based on 3-dimensional analysis of the coronary anatomy. It has also been found to have good correlation and agreement with FFR.6 No prospective studies, however, have compared RFR or QFR with FFR. The aims of this study were to evaluate and compare the ability of RFR and QFR to predict FFR in a prospective sample and, based on our results, to propose a combined algorithm for minimally invasive functional assessment.
Following approval of the study by the research committee, we consecutively included patients scheduled for functional assessment in 3 high-volume hospitals. The physiological parameters requiring an invasive approach were measured using the Abbott Vascular guidewire (Abbott Vascular, USA). RFR was calculated using the dedicated Coroventis AB (Sweden) software program. Hyperemia was then induced to calculate FFR. Angiographic images captured using recommended procedures6 were reconstructed to calculate QFR (Medis, Netherlands).
Pearson correlation analysis was used to assess correlations between QFR, RFR, and FFR. The level of agreement between the 3 indices was analyzed using the Bland-Altman method and the intraclass correlation coefficient. The ability of each index to predict significant stenosis was analyzed using receiver operating characteristic curves with a predefined cutoff value of ≤0.80 for FFR and QFR and ≤0.89 for RFR.
A total of 101 vessels (77 patients) were studied. The mean±SD age of the patients was 69.3±10 years and 70.1% were male. The most common diagnosis was stable angina (40.3%).
The mean percent diameter stenosis based on visual estimation was 54%±14%. Mean FFR was 0.84±0.09 and, based on this index, 30.7% of the vessels had significant stenosis. RFR identified significant stenosis in 51.5% of the vessels and the mean value was 0.88±0.09. Assessment of stenosis by QFR was possible in 89 vessels (88.1%). The mean value was 0.86±0.08 and 27% of the vessels had significant stenosis.
The intraclass correlation coefficients between QFR and FFR and RFR and FFR were 0.92 (95% confidence interval [95%CI], 0.88-0.95) and 0.76 (95%CI, 0.67-0.84), respectively. The mean differences between the indices were 0.04±0.006 for RFR and FFR and 0.01±0.03 for QFR and FFR (figure 1A,B). RFR produced 20 false positive (30.3%) and 1 false negative (3%). By contrast, just 1 of the vessels (1.6%) identified as significant by QFR did not have significant stenosis and 5 (17.9%) of the vessels considered nonsignificant by QFR had an FFR ≤ 0.80 (figure 1C,D).
Agreement, correlation, and ROC curves for QFR and RFR compared with FFR. 95%CI, 95% confidence interval; AUC, area under the curve; FFR: fractional flow reserve; QFR, quantitative flow ratio; RFR, resting full-cycle ratio; ROC, receiver operating characteristic; SD, standard deviation.
Assessment of the diagnostic accuracy of visual estimation to detect FFR with a cutoff of ≤0.80 (stenosis >70% of diameter) showed a sensitivity of 34.4% and a specificity of 87.5%. The respective results for RFR and QFR were 96.7% and 82.15% for sensitivity and 67.7% and 98.36% for specificity (figure 1E). Although QFR and RFR had extreme diagnostic accuracy values of 100% and 84.4%, respectively, for values close to the cutoff point (FFR of between 0.75 and 0.85), their accuracy for values at or below the cutoff point was lower: 80% for QFR and 68.6% for RFR.
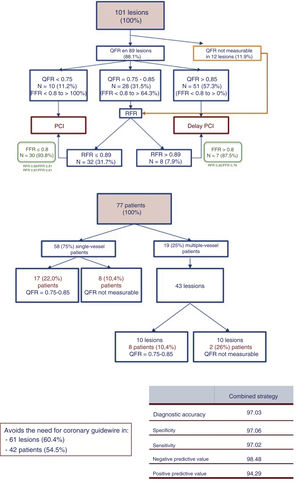
Our proposed combined algorithm-based approach is shown in figure 2. The accuracy of QFR at extreme values would have eliminated the need for a coronary guidewire in 61 lesions (42 patients, 54.5%). RFR should be used for values near the cutoff point and for cases where QFR cannot be measured. The diagnostic accuracy of this combined approach to detect FFR ≤ 0.80 was 97.03%.
This is the first prospective study to compare RFR and QFR with FFR. Our combined approach showed excellent diagnostic accuracy compared with FFR. Apart from overconfidence in the adequacy of visual estimation, the main reasons for not using coronary physiological indices are the need to induce hyperemia1 and difficulties with guidewire manipulation.2 Use of the algorithm shown in figure 2 would have avoided hyperemia induction in 100% of patients and use of a coronary guidewire in more than 50%.
Although our study has significant limitations, such as a lack of comparison with other resting coronary physiological indices and not knowing how consistent these data would be if measured by clinicians with less training in QFR analysis, our approach could be useful for increasing the use of functional assessment of coronary lesions. Further studies are needed to confirm our proposed strategy.
FundingThis project was partially funded by an unconditional grant from the Regional Health Department of Castilla and León (GRS 1728/A/18).