To the Editor,
The number of pacemakers and implantable cardioverter defibrillators implanted each year continues to grow in Spain, due largely to the increased life expectancy of the population in the case of pacemakers and the indications for primary prevention in the case of implantable cardioverter defibrillators.1, 2 Although the incidence of infections associated with implantable cardiac devices is not high, this complication is responsible for increased morbidity and mortality among affected patients. The strategy for achieving the best outcomes is complete removal of the system (electrodes and generator), along with prolonged antibiotic therapy.1 In addition to the general problems faced in pacing-dependent patients, there is also the need for temporary cardiac pacing, at times very prolonged, before implantation of a new system. In most cases, temporary pacing is achieved through transluminal percutaneous placement of a bipolar electrode under radioscopic guidance. The electrode is advanced until good endocardial contact is achieved in the chamber to be paced. This electrode is then connected to a temporary pacing generator. However, the need for prolonged pacing increases the risk of electrode displacement, as well as capture or detection failure, something which may have particularly negative consequences in pacing-dependent patients.
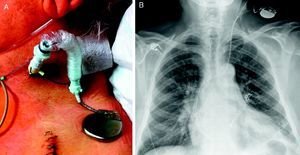
We present the case of a 68-year-old man with a longstanding history of nonischemic cardiomyopathy who received a single-chamber internal defibrillation system in 2007 as primary prevention for sudden cardiac death. The active fixation electrode was implanted in the apex of the right ventricle. At the time of implantation, the patient had very depressed left ventricular systolic function and was in chronic atrial fibrillation. Months after implantation, the patient needed permanent pacing after medical treatment had been progressively optimized. Four years later, the patient showed progressive deterioration in his functional class and replacement of the single-chamber defibrillation system with a defibrillation system with cardiac resynchronization was considered. While awaiting the procedure, the patient presented with an abscess in the region of the generator pocket. The system was completely removed and intravenous antibiotic therapy started to treat the late infectious process prior to implantation of the new system. In view of the complete dependence on pacing, it was decided, before removal, to implant a pacing system that would allow safe, easy, and prolonged physiologic pacing. Thus, with access via the left internal jugular vein and using a short sleeved introducer (Figure 1A), a conventional permanent active fixation pacing electrode was advanced under radiologic guidance and in sterile conditions. The electrode was placed in the septal region of the right ventricle, with an optimum pacing threshold (Figure 1B). The electrode was connected to a permanent sterilized pacemaker generator that had been removed from another patient without signs of infection. The generator was programmed in VVI/R mode at 70 bpm to 120 bpm to allow a more physiologic pacing. The introducer was attached to the skin, the sleeve was attached to the electrode, and the generator was fixed with covering adhesive bandaging to the left supraclavicular region to avoid pulling on the electrode or displacement of the generator. On the following day, the infected system was removed percutaneously without complications. The patient was able to walk from the next day onwards. This situation lasted 21 days while the prescribed antibiotic therapy was completed. After implantation, a defibrillation system with biventricular pacing was implanted, without any complications, and the fixation electrode was removed under radiologic guidance, also without any complications. The patient was discharged without any incidents, and showed a favorable clinical response to the new therapy and did not experience any subsequent complications.
Figure 1. A: Left cervical region where the implanted system can be observed. B: Posteroanterior chest X-ray after removal of the infected system.
The use of active fixation electrodes in permanent pacing to achieve appropriate temporary pacing has the advantage of greater electrode stability and the possibility of placement in different areas of the heart (in this case, the right ventricular septum was chosen to avoid complications on removing the previously implanted electrode from the apex). In addition, the risk of perforation is minimized with the greater flexibility and the possibility of avoiding apical sites. Inadvertent or accidental displacement of the electrode is not uncommon in long-term carriers of provisional pacemakers, and the outcome with an active fixation system when this occurs could be compromised. Thus, particular care should be taken when dressing the wound and in ensuring that the system is stably fixed in the cervical region of the patient. On the other hand, the fact that it can be connected to a permanent pacemaker generator allows for programming of more physiologic pacing modes that help to maintain the patient in a stable clinical condition and allow the patient to walk about without clinical deterioration. Such advantages are particularly desirable in patients who are totally dependent on pacing and who require very prolonged temporary pacing. The small size of the generator is conducive to portability, and this in turn helps ensure that the patient can walk around and has greater mobility in general.
As a precaution, the resterilized pacemaker generators that are used for this purpose, although only ever in contact with the skin of the patient, should come from patients without evidence of infection at the time of switching to minimize the possibility of infection. The greater cost of the active fixation electrode used compared to the usual temporary pacing electrodes is compensated by the fact that the patient does not require admission to hospital in a unit with facilities for close patient monitoring.
This technique should be considered in patients who will require prolonged temporary pacing for any reason,3 particularly those who are pacing-dependent.
Corresponding author: maapalomares@secardiologia.es