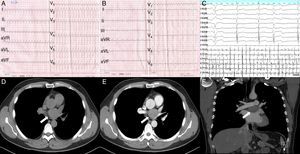
We report the case of a 38-year-old man with a 6-month history of paroxysmal palpitation and presyncope that was refractory to medical therapy. He was admitted to our hospital due to spontaneous onset of palpitation and recurrent presyncope with sweating and nausea. On admission, 12-lead electrocardiography revealed atrial tachycardia (cycle length, 280ms) with 1:1 or 2:1 ventricular conduction (Figure 1A and 1B). Atrial fibrillation was documented in another electrocardiogram and repeatedly converted to atrial tachycardia in the subsequent electrocardiogram. Transthoracic echocardiography found no abnormality. However, because an atrial fibrillation ablation procedure was planned, we performed transesophageal echocardiography to exclude the presence of atrial thrombus. This imaging study revealed a suspicious mass between the aortic root and left atrial roof. Chest computed tomography showed a 30 × 38-mm contrast-enhanced intrapericardial mass between the aortic root and left atrial roof that compressed the left atrium and left superior pulmonary vein (Figure 1D-1F). Computed tomography scans of the abdomen, pelvis, and head found no signs of distant metastasis. Serum tumor marker testing revealed neuron specific enolase of 29.52μg/L (normal range, 0.0-16.30) and CA-724 of 11.81 KU/L (normal range, 0.0-6.90).
Perioperative manifestations of ECG and chest CT images of intrapericardial leiomyoma. A and B: Preoperative 12-lead ECG showed atrial tachycardia (cycle length, 280ms) with 1:1 (A) or 2:1 (B) ventricular conduction. C: Intraoperative epicardial mapping revealed atrial fibrillation. D: The plain CT scan showed an intrapericardial soft tissue mass (arrow) between the ascending and descending aorta. E: Iodine-contrast CT showed a well-circumscribed mass (arrow) with mild enhancement compressing the left pulmonary vein. F: Coronal reconstruction revealed that the mass (arrow) was located between the right pulmonary artery and left atrial roof. CT, computed tomography; ECG, electrocardiogram.
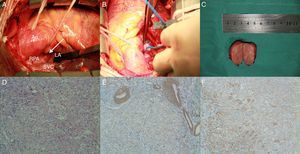
Because the possibility of malignancy could not be excluded, surgical resection of the tumor was recommended for definitive tissue diagnosis. Operative exploration was performed via median sternotomy. During the operation, a solid, well-encapsulated mass was identified in the transverse sinus of the pericardium, attached to the roof of the left atrium (Figure 2A). The tumor was completely removed using a combination of sharp and blunt dissection and was diagnosed as a paraganglioma using fast-frozen pathological examination. The atrial tachycardia spontaneously degenerated into atrial fibrillation again during resection of the tumor (Figure 1C and Figure 2B). However, tumor removal failed to normalize the electrocardiogram and the sinus rhythm was restored using synchronized cardioversion. Immunohistochemical examination of the tumor confirmed the diagnosis of leiomyoma, which was potentially malignant or low-grade (Figure 2C-2F). Postoperatively, the patient underwent 6 cycles of radiotherapy after consultation with an oncologist. He was discharged uneventfully. There has been no recurrence of the arrhythmia or tumor during the 4 years after the surgery.
Intraoperative and histological views of intrapericardial leiomyoma. A: Intraoperative photograph of the leiomyoma (arrow). B: Epicardial mapping with a Lasso catheter. C: The bisected mass was well circumscribed and encapsulated. The cut surface was tan to grey and felt fleshy. D: The tumor was dominated by sheet-like epithelioid cells with abundant eosinophilic or clear cytoplasm and round nuclei with inconspicuous nuclei, intermingled with spindle cells arranged in fascicle patterns (hematoxylin-eosin stain; magnification, ×100). E and F: Immunohistochemical staining showed that the tumor cells were diffusely positive for smooth muscle actin (E) and desmin (F) but negative for HMB45 and melan-A (magnification, ×100). Ao, aorta; LA, left atrium; RPA, right pulmonary artery; SVC, superior vena cava.
This case report highlights the occurrence of atrial tachyarrhythmia as the first symptom of intrapericardial tumor. A distortion by the tumor of the normal anatomy of the heart or pulmonary veins is a rare cause of atrial tachyarrhythmia.1 In our patient, the atrial tachyarrhythmia was most likely due to compression of the left atrial roof and left superior pulmonary vein because the symptoms completely relieved after tumor removal. The proposed mechanism might involve tumor compression or infiltration of normal myocardial cells favoring micro-reentry formation.
Transesophageal echocardiography is advised prior to ablation in patients with atrial fibrillation because it can identify the presence of thrombosis. In the present case, the transthoracic echocardiography results were normal but transesophageal echocardiography revealed a suspicious mass. Accordingly, chest computed tomography was indicated and intracardiac reconstruction was used to confirm the tumor location and the surrounding anatomy. A previous study showed that it is difficult to differentiate extracardiac tumors from intracardiac tumors with echocardiography.2 Multimodality imaging combining cardiac computed tomography and magnetic resonance imaging is recommended for the differential diagnosis of intrapericardial masses.
Leiomyoma is an extremely rare intrapericardial tumor that probably arises from vascular smooth muscle. The first case was reported by Horton et al.3 in 2006 and was reported to be a large pericardial effusion without arrhythmia. To our knowledge, this is the second reported intrapericardial leiomyoma and the first case of an intrapericardial tumor causing spontaneous atrial tachyarrhythmia. Although it is unusual and lacking in specific manifestations, leiomyoma should be considered in the differential diagnosis of intrapericardial tumors.
In conclusion, primary intrapericardial tumors are rare but should be considered as a possible cause of atrial arrhythmia.
This work was supported by the Priority Academic Program Development of Jiangsu Higher Education Institutions [JX10231801].