Cardiovascular disease is still one of the main causes of morbidity and mortality in industrialized countries. Coronary disease causes 5 million hospital admissions for acute myocardial infarction,1 and heart failure (with a prevalence of 6.8% in the population older than 45 years) is the first cause of hospitalization in patients older than 65 years in Spain.2 Therefore, both diseases involve high health care resource utilization and many cardiology hospital admissions, with wide variation in length of hospital stay. Determining which factors prolong hospitalization is important when planning occupation needs and strategies to avoid admissions.
The objective of this study was to determine the factors that could predict prolonged hospitalization (PH) in the cardiology ward of our hospital. To do this, we conducted a prospective, observational study that analyzed 1650 patients who were consecutively admitted to the cardiology ward of another hospital between August 2011 and January 2012, referred by the emergency department, the coronary unit, or another department. We excluded patients with scheduled admissions for diagnostic and/or therapeutic procedures. We collected demographic and clinical variables and the diagnostic tests performed while the patients were in hospital. The mean hospital stay was defined as the interval (days) between hospital admission and the discharge date. To avoid extreme values, patients who were below the 5th percentile or above the 95th percentile were excluded from the mean hospital stay (n=83). PH was defined as a hospital stay longer than 4 days. The categorical variables were expressed as percentages and the quantitative variables as mean (standard deviation); comparisons were made with the χ2 test, Fisher's exact test or Student's t test, respectively. The predictors of PH were determined with a univariable analysis, and statistically significant variables were included in the multivariable binary logistic regression analysis expressed as the odds ratio. The statistical analysis was performed with the IBM SPSS Statistics 2.0 program (Chicago, Illinois, United States). P values of <.05 were considered statistically significant.
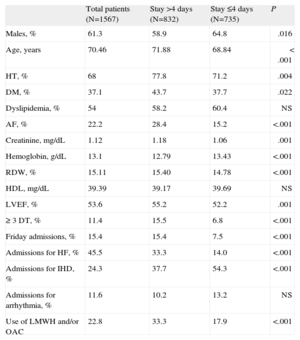
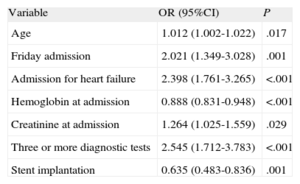
The total number of patients included was 1567 and 61.3% (n=961) were male, with a mean age of 73 (12.8) years. The mean duration of admission was 5.3 (3.4) days and the median [interquartile range] was 5 [3-8] days; 713 patients (45.5%) were admitted for ischemic heart disease; 380 (24.3%) for heart failure; 182 (11.6%) for bradycardia or tachycardia; 96 (6.1%) for chest pain; 65 (4.1%) for syncope; and the remaining 131 (8.36%) for other causes such as endocarditis, myocarditis, or pericardial disease. More than half of the patients (53.1%) were in hospital for >4 days (PH). The baseline characteristics and differences according to whether hospitalization was prolonged or not are summarized in Table 1. In the multivariable analysis, age, admission for congestive heart failure, creatinine and hemoglobin levels at admission, the performance of 3 or more diagnostic tests, and admission on a Friday rather than on other days of the week were independent PH predictors, whereas the performance of coronary angioplasty was a a protective factor (Table 2).
Characteristics of the Sample at Baseline and According to the Period in Hospital
| Total patients (N=1567) | Stay >4 days (N=832) | Stay ≤4 days (N=735) | P | |
| Males, % | 61.3 | 58.9 | 64.8 | .016 |
| Age, years | 70.46 | 71.88 | 68.84 | < .001 |
| HT, % | 68 | 77.8 | 71.2 | .004 |
| DM, % | 37.1 | 43.7 | 37.7 | .022 |
| Dyslipidemia, % | 54 | 58.2 | 60.4 | NS |
| AF, % | 22.2 | 28.4 | 15.2 | <.001 |
| Creatinine, mg/dL | 1.12 | 1.18 | 1.06 | .001 |
| Hemoglobin, g/dL | 13.1 | 12.79 | 13.43 | <.001 |
| RDW, % | 15.11 | 15.40 | 14.78 | <.001 |
| HDL, mg/dL | 39.39 | 39.17 | 39.69 | NS |
| LVEF, % | 53.6 | 55.2 | 52.2 | .001 |
| ≥ 3 DT, % | 11.4 | 15.5 | 6.8 | <.001 |
| Friday admissions, % | 15.4 | 15.4 | 7.5 | <.001 |
| Admissions for HF, % | 45.5 | 33.3 | 14.0 | <.001 |
| Admissions for IHD, % | 24.3 | 37.7 | 54.3 | <.001 |
| Admissions for arrhythmia, % | 11.6 | 10.2 | 13.2 | NS |
| Use of LMWH and/or OAC | 22.8 | 33.3 | 17.9 | <.001 |
AF, atrial fibrillation; DM, diabetes mellitus; DT, diagnostic tests; HDL, high-density lipoprotein; HF, heart failure; HT, hypertension; IHD, ischemic heart disease; LVEF, left ventricular ejection fraction; LMWH, low molecular weight heparin; NS, non significant; OAC, oral anticoagulants; RDW, red blood cell distribution width.
Independent Predictors of Prolonged Hospitalization (>4 Days) (Multivariable Analysis, Logistic Regression)
| Variable | OR (95%CI) | P |
| Age | 1.012 (1.002-1.022) | .017 |
| Friday admission | 2.021 (1.349-3.028) | .001 |
| Admission for heart failure | 2.398 (1.761-3.265) | <.001 |
| Hemoglobin at admission | 0.888 (0.831-0.948) | <.001 |
| Creatinine at admission | 1.264 (1.025-1.559) | .029 |
| Three or more diagnostic tests | 2.545 (1.712-3.783) | <.001 |
| Stent implantation | 0.635 (0.483-0.836) | .001 |
95%CI, 95% confidence interval; OR, odds ratio.
The mean hospital stay in our ward was within the range published by other articles.3 Our results, like those reported for similar environments,4 show that hospital stay is longer in older patients with more comorbidity than in younger patients with fewer concomitant diseases. Importantly, the performance of coronary angioplasty was a protective factor, due to a tendency to perform percutaneous revascularization earlier and more conservatively, which can reduce hospital stay and its associated complications.
Some of the factors related to PH in cardiology, such as age, creatinine, and hemoglobin at admission, are inherent to the population admitted to hospital and cannot be modified, but others, such as Friday admissions, admissions for heart failure, early revascularization strategies, and the performance of multiple tests can be taken into account when planning policies to reduce length of hospital stay. A change in working hours could be proposed (eg, making Saturdays an ordinary working day) as well as encouraging the creation and promotion of heart failure units with resources, or accelerating the performance of diagnostic techniques (or performing them on an outpatient basis), which could reduce the PH rate. One of the limitations of our study is its observational design and therefore data could only be recorded while the patients were in hospital, without correlating PH and the complications of follow-up.