The prognosis of heart transplantation (HT) has improved in the last decade,1 but outcomes could still be improved. In the setting of HT, the detection of acute rejection (AR) using non-invasive methods remains a challenge. Echocardiography is only useful for detecting AR when performed by an expert in HT,2 and biomarkers such as natriuretic peptides are not sufficiently reliable to replace endomyocardial biopsy (EMB) in the diagnosis of AR.3 Cardiac troponin is an early marker of myocardial damage and highly sensitive methods have recently been described to measure cardiac troponin concentrations.4 High-sensitivity troponin T (hs-TnT) could be a useful marker of the minor myocardial necrosis associated with AR after HT.
This study analyzed the effectiveness of measuring hs-TnT concentrations to diagnose or rule out AR in 73 HTs conducted in 2 hospitals. The EMBs were performed and 234 blood samples were prospectively obtained (113 and 121 samples at each hospital) on the same day. The EMB was performed in 1 hospital within the first year after HT, in the second hospital within 6 months, and then as needed. Before the results of the hs-TnT studies were known, acute rejection was diagnosed when the EMB was interpreted as grade ≥ 2R according to the criteria of the International Society for Heart and Lung Transplantation (ISHLT).5 The hs-TnT concentrations were analyzed centrally using the electrochemiluminescence immunoassay method (Roche Diagnostics; Basel, Switzerland). The usefulness of hs-TnT to rule out AR was assessed by calculating the area under the receiver operating characteristic (ROC) curve and its 95% confidence intervals (95%CI). The hs-TnT values were standardized by log transformation. The odds ratio (OR) of the mixed-effects logistic regression model is shown. Ten EMBs were considered uninterpretable and were excluded from the study. Of the remaining 224 EMBs, 183 were obtained within the first 3 months of HT, 25 were obtained between 3 months and 12 months, and 16 were obtained on the basis of suspected late AR. The study was approved by the respective ethics committees and informed consent was obtained from the patients.
Table 1 shows the clinical characteristics of the patients. In total, 16 EMBs were interpreted as ISHLT grade ≥ 2R (7%). The hs-TnT concentrations were higher in EMBs with ISHLT grade ≥ 2R (mean, 164 [SD, 3.3] ng/L) than when there was no AR (mean, 74 [SD, 3.7] ng/L) (P<.05). After excluding AR, a significant inverse correlation was maintained between hs-TnT concentrations and time after HT (R=-0.49; P=.0001). The ROC curve of hs-TnT for detecting AR was 0.682 (95%CI, 0.54-0.81; P=.01). A hs-TnT concentration<17 ng/L ruled out AR with a sensitivity and a negative predictive value of 100%, but a specificity of 13% (Table 2); there were 29 true negatives for AR with hs-TnT<17 ng/L. In a mixed-effects logistic regression model, the hs-TnT values were log transformed and showed an OR=1.58 (95%CI, 1.06-2.37; P=.026).
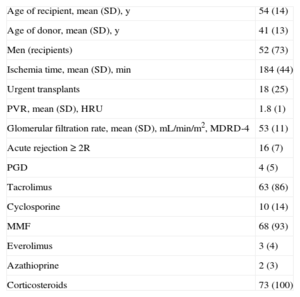
Clinical Characteristics of the 73 Heart Transplantation Recipients and Donors
| Age of recipient, mean (SD), y | 54 (14) |
| Age of donor, mean (SD), y | 41 (13) |
| Men (recipients) | 52 (73) |
| Ischemia time, mean (SD), min | 184 (44) |
| Urgent transplants | 18 (25) |
| PVR, mean (SD), HRU | 1.8 (1) |
| Glomerular filtration rate, mean (SD), mL/min/m2, MDRD-4 | 53 (11) |
| Acute rejection ≥ 2R | 16 (7) |
| PGD | 4 (5) |
| Tacrolimus | 63 (86) |
| Cyclosporine | 10 (14) |
| MMF | 68 (93) |
| Everolimus | 3 (4) |
| Azathioprine | 2 (3) |
| Corticosteroids | 73 (100) |
SD, standard deviation; MDRD, Modification in Diet in Renal Disease Study Group; MMF, mycophenolate mofetil; PGD, primary graft dysfunction; PVR, pulmonary vascular resistance.
Data are expressed as No. (%) or mean (standard deviation).
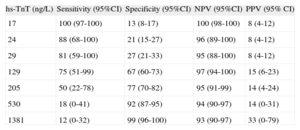
Sensitivity, Specificity, and Negative and Positive Predictive Values of Different Hs-Tnt Concentrations to Diagnose or Rule Out Acute Rejection After Cardiac Transplantation
| hs-TnT (ng/L) | Sensitivity (95%CI) | Specificity (95%CI) | NPV (95%CI) | PPV (95% CI) |
| 17 | 100 (97-100) | 13 (8-17) | 100 (98-100) | 8 (4-12) |
| 24 | 88 (68-100) | 21 (15-27) | 96 (89-100) | 8 (4-12) |
| 29 | 81 (59-100) | 27 (21-33) | 95 (88-100) | 8 (4-12) |
| 129 | 75 (51-99) | 67 (60-73) | 97 (94-100) | 15 (6-23) |
| 205 | 50 (22-78) | 77 (70-82) | 95 (91-99) | 14 (4-24) |
| 530 | 18 (0-41) | 92 (87-95) | 94 (90-97) | 14 (0-31) |
| 1381 | 12 (0-32) | 99 (96-100) | 93 (90-97) | 33 (0-79) |
95%CI, 95%CI confidence interval; hs-TnT, high sensitivity troponin T; NPV, negative predictive value; PPV, positive predictive value.
This study suggests that hs-TnT concentrations < 17 ng/L may rule out AR with a sensitivity and negative predictive value of 100% (Table 2) and without obtaining false negatives. A noninvasive method to rule out AR may be useful in patients with contraindications to EMB and in those with insufficient material for histopathological study. Furthermore, a negative predictive value of 95% was observed at hs-TnT concentrations < 29 ng/L, which indicates that the probability of AR is low at hs-TnT concentrations of 17 ng/L to 29 ng/L. These concentrations are very close to the 99th percentile of the reference marker (14 ng/L) and to the upper limit of the confidence interval (24.9 ng/L) of this percentile, respectively (percentile reference range for hs-TnT; Roche Diagnostics package insert). Moreover, the histological detection of AR is limited because it does not distinguish between active and residual myocytolysis.
The study data suggest that the measurement of hs-TnT concentrations can complement the histopathological diagnosis of AR. Thus, an ISHLT grade ≥ 2R associated with low hs-TnT concentrations may suggest a low or mild focal phenomenon; in contrast, high hs-TnT concentrations could indicate a more diffuse and active rejection and therefore more severe AR. The study also shows that in the first months after HT, the high hs-TnT concentrations decrease in inverse proportion to time after HT, but may remain elevated for more than 6 months. This phenomenon may be explained by the high hs-TnT concentrations before HT, by myocardial damage due to the transplant procedure, or by subclinical rejection undetectable by biopsy but detectable by hs-TnT concentrations. The low specificity of hs-TnT for detecting AR has been described in another study that demonstrated its low reliability for diagnosing AR.6
In conclusion, the results suggest that the determination of hs-TnT concentrations may be useful to rule out AR, especially if concentrations are < 17 ng/L.
FUNDINGThe study was funded by the Spanish Society of Cardiology and the Ministry of Health (Red de Investigación Cardiovascular, Instituto de Salud Carlos III).
The authors would like to thank Andreu Ferrero for assisting with the statistical analysis, Silvia Terzán and Tere Mir for measuring hs-TnT concentrations, and Dr José Ramírez (Hospital Clínic) and Dr José Sancho (Hospital de la Santa Creu i Sant Pau) for interpreting the myocardial biopsies.