We present the case of a patient with vasospastic angina and postural orthostatic tachycardia syndrome (POTS), an association that has not been previously described.
A 49-year-old woman was admitted for typical angina, without toxic habits, and with a history of high blood pressure and dyslipidemia, for which she was receiving treatment. An echocardiogram ruled out structural heart disease. Myocardial perfusion scintigraphy showed mild ischemia in the anterior wall, and medical treatment was initiated.
A few months later, the patient was admitted for progressive angina with transient ST-elevation in the anterior wall. Coronary catheterization showed no coronary lesions. Acetylcholine administration showed severe vasospasm of the left coronary tree, which was clinically and electrically positive and underwent remission with intracoronary nitrates. Consequently, a provisional diagnosis of vasospastic angina was made based on standardized international diagnostic criteria.1
During the following years, the patient was often readmitted for refractory angina. Given the severity of the symptoms and the electrical changes, she underwent several coronary catheterisation procedures, without evidence of coronary disease. For this reason, vasodilator treatment was sequentially increased using nitrates and nondihydropyridine calcium antagonists.
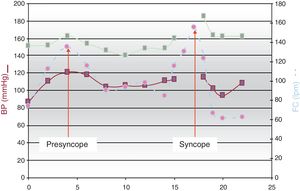
Subsequently, the patient began to develop syncope when standing, which gradually became more frequent and hindered basic activities, such as using the restroom. A 24-hour Holter showed a sinus tachycardia episode at 140 bpm during mild effort. The tilt table test was positive, showing syncopal tachycardia without hypotension, compatible with POTS (Figure 1), although the vasodilator medication almost certainly enhanced the tachycardia response. We attempted to suspend the nitrates to reduce the tachycardia, but this attempt was unsuccessful due to the worsening of the angina.
Catecholamines were determined by a 24-hour urine test and in plasma in decubitus. Values were within the normal range. However, plasma values after 5minutes of standing (with presyncope and tachycardia at 180 bpm) were very high: noradrenaline, 1797 ng/L (normal range, 165-460 ng/L) and adrenaline, 357 ng/L (normal range, 30-90 ng/L). Detailed physical examination ruled out signs of disorders that may occur with orthostatic intolerance, such as Ehlers-Danlos syndrome. That patient had no family history of POTS.
The patient developed frequent syncopes, always while standing, which compelled her to use a wheelchair. Simultaneously, she had New York Heart Association (NYHA) functional class III effort dyspnea and orthopnea, without associated structural heart disease. Catheter-induced coronary vasospasm did not lead to mitral regurgitation or increased pulmonary pressures. However, cardiopulmonary ergometry showed tachycardia and desaturation at 30seconds with hyperlactatemia.
These results were considered secondary to POTS. Thus, clonidine and venlafaxine treatment were started but discontinued due to intolerance and ineffectiveness, respectively. Finally, we decided to increase the blocker drugs, and an improvement was achieved by using a combination of diltiazem 60mg/12h and ivabradine 7.5mg/12h. Due to the recurrence of angina, transdermal nitrate 15mg at night, isosorbide mononitrate 30mg during the day, and sublingual nitroglycerin on demand were maintained. We raised the possibility of cardiac rehabilitation, which the patient rejected due to logistics.
This treatment led to marked improvements that allowed her to carry out her daily activity (walking and standing) without syncopes, with sporadic anginal episodes, and with a clear decrease in effort dyspnea (NYHA Ib).
POTS is defined as an increase in heart rate of more than 30 bpm in the absence of orthostatic hypotension when standing, and is considered to be due to overcompensation by a physiological mechanism. This patient probably had an excessive tachycardia response due to the vasodilator treatment; there are no specific POTS criteria in these circumstances, and so they are known as “facilitated POTS”.
The prevalence of POTS is 0.2% in the general population and the incidence is higher in women (ratio 5:1). Symptoms worsen with standing and the clinical signs and symptoms vary considerably; syncope occurs in approximately 30% of cases (mechanism unknown). Decreased functional class secondary to tachycardia has also been described.
Its pathophysiology is complex and remains uncertain, although there are several theories referring to: hypovolemia and renin-angiotensin-aldosterone system abnormalities; a hyperadrenergic state (with increased catecholamines upon standing)2; peripheral microcirculation abnormalities3; peripheral dysautonomia; and cardiac deconditioning and atrophy.
The response of our patient to the tilt table test and increased levels of catecholamines upon standing were diagnostic of POTS. Hypoxia and increased lactate levels were also documented during ergometry due to excessive early tachycardia, with no alternative cause of dyspnea being demonstrated.
Although not previously described in the literature, the association between POTS and coronary vasospasm is striking. However, the known association between POTS and peripheral endothelial dysfunction in relation to nitric oxide system abnormalities3 could also account for coronary vasospasm. The intensity of the vasodilator treatment prescribed for vasospasm could well have worsened the tachycardia and the symptoms associated with POTS, which may have made it difficult to achieve therapeutic balance.
General treatment comprises lifestyle measures (abundant hydration, sodium intake) and cardiac rehabilitation programs. Regarding pharmacological treatment, the usefulness of fludrocortisone, low-dose propranolol,4 and antiadrenergics (clonidine or alpha-methyldopa) or ivabradine have been described; however, norepinephrine reuptake blockers should be avoided. Ablation of the sinus node is not recommended.
This patient did not tolerate antiadrenergics and the use of beta-blockers was rejected because of the severity of vasospasm. We emphasize that the refractory tachycardia compelled the combined use of diltiazem and ivabradine. Although this combination is not recommended in principle, the patient had good tolerance and clinical response.
In conclusion, we present a case of vasospastic angina associated with probable POTS. Pharmacological treatment was complex because of interactions between the pathophysiology and treatment of the 2 conditions.