Percutaneous closure of the left atrial appendage (LAA) is an accepted procedure for stroke prevention in patients with atrial fibrillation. In patients with heart diseases eligible for percutaneous intervention, LAA obliteration during the same procedure may be particularly beneficial, in view of the clinical profile and high comorbidity of these patients. Transcatheter treatment of concomitant cardiac conditions is emerging as a possible strategy to improve the clinical outcomes of the procedure.
We describe the case of a patient with permanent atrial fibrillation and ventricular septal defect (VSD) following surgery for aortic valve replacement who underwent simultaneous transcatheter closure of the VSD and LAA, as well as the case of a patient with chronic atrial fibrillation and severe symptomatic aortic stenosis who was successfully treated by transfemoral aortic valve implantation (TAVI) and percutaneous LAA closure during the same procedure.
The first patient was a 77-year-old woman with hypertension, dyslipidemia, chronic renal failure, and repeated transient ischemic attacks who had chronic atrial fibrillation plus several episodes of gastrointestinal bleeding; she was also receiving acenocoumarol therapy. The patient had undergone aortic valve replacement 12 years earlier. Due to progressive degeneration of the mechanical prosthesis, she required a new operation for aortic valve replacement. A decision was made to implant a 19-mm Carpentier-Edwards PERIMOUNT Magna Ease (Edwards Lifesciences Corporation, Irvine, California, United States) bioprosthesis, with discontinuation of anticoagulant therapy to be considered during follow-up. After the surgery, she experienced complete atrioventricular block that required implantation of a single-chamber permanent pacemaker. Before discharge, a VSD with a diameter of 6mm was visualized in the perimembranous area; the peak interventricular gradient was 85mmHg and clinical tolerance was initially good; therefore, we decided to adopt a conservative approach. One month later, the patient was readmitted for heart failure.
The case was discussed in a medical-surgical session, and a decision was made to perform percutaneous closure of the VSD and LAA in the same procedure.
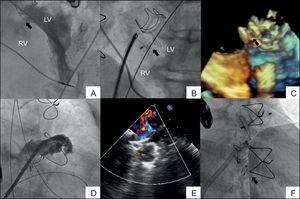
Both femoral veins and the left femoral artery were cannulated, and an initial left ventriculography (Figure 1A) showed a VSD in the perimembranous area, with preserved left ventricular systolic function. A straight-tipped hydrophilic guidewire was advanced using a retrograde approach through the aortic prosthesis and was passed through the VSD to the right atrium, with loop snare in the inferior vena cava and removal of the end through the venous introducer, thus creating an arteriovenous loop. Transseptal puncture was then performed, leaving the medium guidewire in the LAA. The delivery sheath was subsequently advanced from the femoral vein to the left ventricle (Figure 1B), and an 8-mm Amplatzer Muscular VSD Occluder (St. Jude Medical, St. Paul, Minnesota, United States) was implanted, with good disc apposition and no residual shunt as assessed by transesophageal echocardiography (Figure 1C).
A–C: Percutaneous closure of the ventricular septal defect. A: Left ventriculography showing the size and location of the ventricular septal defect (arrow). B: Amplatzer occluder implanted in the defect (arrow) visualized by fluoroscopy. C: 3-Dimensional transesophageal echocardiography. D–F: Percutaneous closure of the left atrial appendage. D, Selective left atrial angiography. E: Transesophageal echocardiography image of the device and complete left atrial appendage occlusion with no color Doppler flow. D: Final angiographic image of both devices. LV, left ventricle; RV, right ventricle.
Finally, percutaneous closure of the LAA was performed using a 22-mm Amplatzer Cardiac Plug® (AGA Medical Corporation; Plymouth, Minnesota, United States), with good final outcome as observed by angiography and transesophageal echocardiography (Figures 1D-F). The patient was discharged 2 days later, with dual antiplatelet therapy; 4 months later, she remains asymptomatic and is receiving acetylsalicylic acid therapy.
The second patient was a 91-year-old man with hypertension, dyslipidemia, chronic renal failure, and permanent atrial fibrillation who was admitted for congestive heart failure and hemoptysis. He had experienced prior episodes of gastrointestinal bleeding and was receiving acenocoumarol and rivaroxaban therapy; however, endoscopic studies showed no pathologic findings. Transthoracic echocardiography showed severe aortic stenosis, moderate pulmonary hypertension, and normal left ventricular systolic function. Coronary angiography revealed diseases in 2 secondary vessels (second diagonal and first obtuse marginal).
The case was assessed by the Heart Team, which decided to perform transfemoral transcatheter aortic valve implantation (TAVI) and percutaneous closure of the LAA during the same procedure.
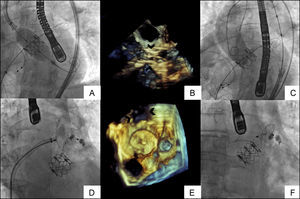
The left femoral artery was punctured, and the contralateral artery was accessed as previously described.1 Both femoral veins were accessed by transseptal puncture, and a 0.035-inch Amplatzer medium guidewire was advanced to the left upper pulmonary vein and a temporary pacing lead was advanced to the right ventricular apex. Based on transesophageal echocardiography images and aortography, it was decided to proceed with direct implantation (no prior valvuloplasty) of a 26-mm Edwards SAPIEN XT valve (Edwards Lifesciences Corporation, Irvine, California, United States); the valve was properly expanded (Figures 2A-B) with no perivalvular regurgitation (Figure 2C). The Novaflex delivery system was withdrawn, an 18-Fr introducer was left in the right femoral artery, and an elective injection was then performed on the LAA through a 13-Fr Amplatzer sheath (Figure 2D). Based on an analysis of 2 orthogonal views and the transesophageal echocardiography images, a 28-mm Amplatzer Cardiac Plug® was implanted for LAA percutaneous closure. Finally, percutaneous closure of the femoral access was performed using Prostar XL (Abbott Laboratories. Abbott Park, Illinois, United States), with adequate hemostasis.
A–C: Implant of 26-mm Edwards–SAPIEN XT valve. A: Direct implantation of the prosthesis with good expansion verified by fluoroscopy. B: 3-Dimensional transesophageal echocardiography. C: No periprosthetic aortic regurgitation in final aortography. The arrows show the stent of the prosthesis. D–F: Implant of left atrial appendage closure device with 28-mm Amplatzer Cardiac Plug®. D: Fluoroscopy-guided placement of the device. E: 3-Dimensional transesophageal echocardiography. F: Final image of both devices.
To date, isolated cases have been reported that combined several sequentially-performed structural interventional procedures, including deferred closure of the LAA after TAVI2 or after mitral valve repair using the MitraClip system (Abbott Laboratories. Abbott Park, Illinois, United States).3 However, simultaneous transcatheter treatment of several heart conditions, including percutaneous LAA closure combined with other structural interventional procedures, could be particularly beneficial, as it allows immediate suspension of anticoagulation therapy and reduces the risk of bleeding after the procedure.
The use of combined percutaneous procedures in certain cases may offer some clinical advantages and improve the overall outcome of the procedure, while also providing cost savings.