Keywords
INTRODUCTION
Fistulas between the internal mammary artery (IMA) and the pulmonary arteries are uncommon vascular abnormalities.1 Most individuals with such abnormalities are usually asymptomatic and the fistula is only detected in the physical examination because of a characteristic continuous murmur.2
For diagnosis and localization of the fistula, aortography and selective angiography of the IMA are used.1 In view of the possible of circulatory overload, degeneration of the arterial wall, infection, traumatic rupture or other complications,3 surgical closure of the defect, as described in the 20 cases reported in the literature, might be indicated.
We think our contribution is of interest because of the novelty of catheter closure of a mammary-pulmonary fistula with double arterial supply using a technique that combines use of coils and an Amplatzer Duct Occluder (ADO) device.
CASE STUDY
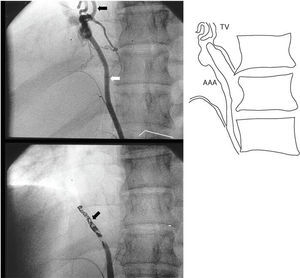
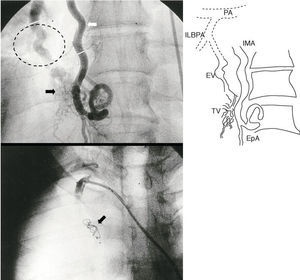
A 32-year-old man, who played sports regularly, presented with continuous murmur discovered by chance in his company's medical check-up. He had no cardiovascular risk factors, relevant clinical history, chest trauma or prior surgery. Chest x-ray showed no significant findings and, according to the electrocardiogram (ECG), he had sinus rhythm with a QRS axis of 60º, without increased cavity dimensions, or rhythm or conduction disorders. Transthoracic echocardiography revealed limited dilation of the right chambers without pulmonary hypertension, as the only significant finding. Thoracoabdominal computed tomography (CT) showed a possible vascular fistula between the right IMA and an aberrant artery that connected the abdominal aorta and the inferior lobar branch of the right pulmonary artery. Although the patient was asymptomatic, it was decided to close the defect because of the risk of chest trauma associated with playing sports. The procedure was carried out by retrograde puncture of the right femoral artery. A large 5 mm aberrant artery next to the celiac trunk was selectively probed. The aberrant artery flowed towards the anterior phrenic and right medial region, to give flow to a vascular tangle neoformation 4 cm in diameter. A 6-mm efferent vessel from this tangle drained the inferior right lobar pulmonary artery. Next, the right mammary artery was selectively probed. It was found to be well developed, with a diameter of 6 mm. This artery, before becoming the epigastric artery, gave rise to several afferent branches to the vascular tangle found in the phrenic region with drainage through to the efferent vessel mentioned above. To close the aortic-mammary-pulmonary fistula, the aberrant aortic artery was selectively probed, and 20 MWCE-135HILAL (COOK) coils, 5 mm long by 4 mm in diameter, were placed to achieve complete vessel occlusion (Figure 1). Next, a 6-Fr sheaf was placed in the mammary artery and an ADO device of 6-8 mm and a Flipper PDA5 coil of 8 mm diameter with 5 turns were implanted, and the vessel closed completely (Figure 2). The difference in arterial oxygen content between the right ventricle and the right pulmonary artery was 1.3% by volume, and the pressures in the smaller circuit were normal. Final aortography showed closure of the double supply by occlusion of both vessels. Prophylactic antibiotics were administered for 7 days. Chest contrast CT was performed at 2 months and at one year post procedure. Both showed that the artery-artery fistula had disappeared.
Fig. 1. Top: selective injection showing an aberrant abdominal aortic artery (AAA) (white arrow) which flows towards the phrenic region to a vascular neoformation (NV) (black arrow). Bottom: complete occlusion after placement of 20 coils (arrow) in the aberrant artery.
Fig. 2. Top: selective probing of the highly developed right internal mammary artery (IMA) (white arrow) and of several branches the vascular tangle (black arrow). The efferent vessel (EV) (circle) flows from the tangle and drains into the inferior lobar branch of the pulmonary artery (ILBPA). Bottom: closure of large IMA with Amplatzer Duct Occluder device (arrow). EpA indicates epigastric artery; PA, pulmonary artery; NV, vascular neoformation.
DISCUSSION
Mammary artery-to pulmonary artery fistula is a rare malformation--we could only find 20 reports after an exhaustive literature search. The first case of mammary artery-to pulmonary artery fistula was published by Burchell and Clagett,2 of the Mayo Clinic, in 1947. These malformations can be classified into 3 broad groups according to their anatomical connections1: a) those derived from the proximal part of the IMA that connect with the internal mammary vein, the vena cava or the innominate vein; b) those that connect the middle third of the IMA with the pulmonary circulation, and c) those that connect the distal third with the vitelline veins. Other shunts between systemic arteries and pulmonary arteries may originate from intercostal, bronchial, pericardial, pericardiophrenic, lateral thoracic and esophageal arteries, or from anomalous branches of the aorta4,5 (as in our case).
These fistulas may be congenital or acquired from inflammatory,5-7 neoplastic,8 or traumatic4,9 lesions. Congenital fistula has been described in association with other anomalies such as the tetralogy of Fallot,10 with mitral valve prolapse11 or with sick sinus syndrome.12
Several authors have suggested that congenital fistulas arise because pulmonary capillary vessels and the aorta, which connect systemic and pulmonary circulation in the fetus, fail to regress.13 Congenital fistulas may be apparent at birth but not become functionally active until triggered by external factors such as trauma, infection, inflammation, neoplasia or metabolic disorders.4
These fistulas are usually diagnosed in young people in their teens or twenties. The mean age for diagnosis is 22 years. The youngest patient diagnosed was 7 years old and the oldest was 77 years old. In both these patients, the abnormality was diagnosed by abnormal pulmonary circulation in the chest x-ray. The ratio of men to women with such a fistula is approximately 2:1. Clinical presentation depends partly on the functional repercussion of these fistulas, which is proportional to the size of the implicated vessels and the fistula, and where it is located in relation to the heart. All 20 reported cases, and our patient, had a continuous precordial murmur. This poses the problem of differentiating between patients with such fistulas and those with patent ductus arteriosus,14 coronary artery fistula, rupture of Valsalva sinus, ventricular shunt with aortic valve regurgitation, coarctation of the aorta and arteriovenous fistulas. Chest x-ray, ECG and echocardiography all provide valuable information for differential diagnosis, but in this case, selective angiography is necessary to establish diagnosis of a fistula between the IMA and the pulmonary artery.1
With time, artery-artery fistulas may cause vessel dilation and symptoms such as congestive heart failure and bacterial endocarditis.11 In view of the small number of cases, surgical indication for this abnormality is not clearly established. Some authors recommend that all patients should undergo surgery because of the risk of rupture, endarteritis and congestive heart failure due to progressive dilation of abnormal vessels. In contrast, other authors, who doubt the long-term effectiveness of surgery for an abnormality that may have a benign natural course, opt for conservative treatment of young patients. Most of the 20 cases reported in the literature underwent surgery with vessel ligation, alone or in association with excision of pulmonary tissue. No deaths were reported during surgery.11
The Amplatzer Duct Occluder has been successfully used in complete closure of arteriovenous fistulas. This device was initially approved for closure of patent ductus arteriosus. The device is self-expandable, and made from nitinol-wire mesh. There is a retainer disk on one face, which is usually 2 mm larger than the diameter of the device. A Dacron mesh facilitates thrombosis and complete closure of the fistula. The main advantages of these devices are that they can be relocated, come in a wide range of sizes, can be placed by a small delivery catheter, have a high rate of complete closure, and are associated with zero mortality. Given the lack of similar reports in the medical literature, we showed the usefulness of this device in association with coils to close a complex artery-artery fistula.
Correspondence: Dr. F.J. Fernández Fernández.
Cordelería, 3, 2.o D. 48013 Bilbao. Vizcaya. España.
E-mail: mariaf@mibbva.com