Keywords
INTRODUCTION
Cardiac catheterization via the radial artery is increasingly frequent due to reduced vascular complications compared to access via the femoral or humeral route.1-3 However, although infrequent, radial access can be associated with the same problems deriving from puncture, hemostasis or guide management, such as hematoma, pseudoaneurysm, arteriovenous fistula, or perforation of the artery.3,4 The main difference to the femoral route is in the treatment indicated, as well as less blood loss via the radial artery. In femoral catheterization, the use of surgery is quite frequent, whereas in the transradial approach, surgical closure or closure with devices is hardly ever done. Even though there is sufficient information in the literature regarding technical details and experience with the transradial approach, there is no published series describing all the complications specific to the technique and the treatment applied. In this paper, we describe our experience at our center, where the radial artery is the route of choice for cardiac catheterization, regarding the management of these types of complications.
PATIENTS AND METHODS
All hemorrhagic complications arising from radial access from January 2001 to October 2003 were reviewed to identify cases where a pseudoaneurysm, fistula or vascular perforation occurred. Hematomas at the site of puncture were excluded from the analysis since conservative treatment is the only approach followed in this situation. In this period there were no cases of serious hematomas in the forearm with compartment syndrome.
Procedure
Starting in January 2001, the radial approach for cardiac catheterization was progressively introduced in our center. Thus, in 2001, 187 (7.4%) out of 2512 procedures were done radially; in 2002, 1178 (39.6%) out of 2975; and in 2003 (until October), 2038 (76.3%) out of 2672. Use of the radial approach also increased gradually in interventions from 7.1% in 2001 to 77.6% in 2003. A 4 Fr introducer was used for diagnostic procedures and a 5 or 6 Fr introducer for therapeutic ones. A minimum dose of 5000 U heparin was administered, and adjusted to 70 U/kg body weight during angioplasties. The arterial introducer was withdrawn immediately after the procedures. A bandage made of a gauze pad and 3 adhesive elastic bands was used for compression. The bandage was kept on for 2 h for diagnostic procedures and for a minimum of 4 h for therapeutic ones. Until October 2002, a clinical review of all patients was done after 15 days. After this date only patients who had complications were reviewed or ones who were included in a prospective study.
RESULTS
Except for cases of mild or moderate hematomas (≤6 cm), we documented 21 (0.06%) cases of hemorrhagic complications, of which 13 were serious hematomas (>6 cm); 5 patients presented perforation of the artery due to the passage of the guide catheter, 2 patients presented arteriovenous fistulas and there was one case of radial pseudoaneurysm. None of the complications occurred after a failed puncture attempt or radial artery catheterization. One patient presented perforation of the artery during catheterization and an arteriovenous fistula in the perforation site at follow-up. This case was recorded as perforation in order to avoid duplication. The general characteristics of the eight cases of fistula, perforation and pseudoaneurysm that required specific treatment are summarized in the Table and are described below.
Simple Hematoma
Diagnosis was made shortly after removing the compression bandage in most patients, and showed an increase in volume and induration of the area next to the puncture site. Treatment consisted of prolonging compression with a gauze pad and elastic bands.
Pseudoaneurysm
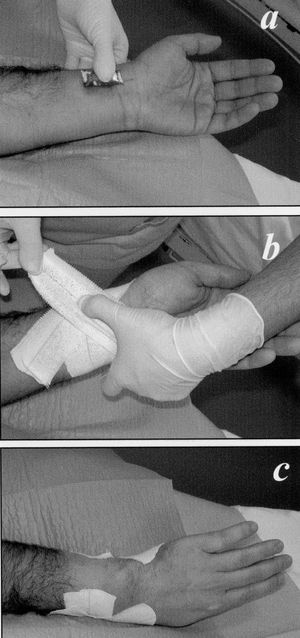
A pseudoaneurysm was identified in the puncture area in just 1 case in the series. The complication arose after angioplasty with stent, done via the right radial artery with a 6 Fr introducer and 6 Fr catheters. No glycoprotein IIb/IIIa inhibitor was used and the heparin dose administered was approximately 70 U/kg. Postangioplasty treatment included aspirin and clopidogrel, but excluded anticoagulants. The following morning the patient presented local swelling, moderate pain and systolic murmur in the puncture area. Pseudoaneurysm was confirmed by Doppler ultrasonography. Oral analgesia was given and a compression bandage applied (Figure 1) for 12 h, which completely resolved the complication.
Fig. 1. Compression done in the cases of arteriovenous fistula or pseudoaneurysm. A: a gauze pad is applied on the puncture point. B: 3 adhesive elastic bands are applied, each approximately 14-cm long. C: the arrangement of the elastic bands should not impede venous return via the dorsal part of the wrist.
Arteriovenous Fistula
The 2 patients who presented arteriovenous fistulas had a very similar clinical picture which started with continuous pain in the puncture area, paresthesias throughout the hand and edema. They presented increased volume of the ipsilateral hand and fremitus when taking the radial pulse. Diagnosis was confirmed by ultrasonography in both cases.
One of the patients was being treated with acenocoumarol (case 3). Treatment included a compression bandage (shown in Figure 1) for 72 h, vertical arm rest, and oral analgesics (tramadol 50 mg/8 h oral). In the first case a fistula persisted for 24 h and the bandage was applied again while surgery was being planned. Two days later closure was verified with Doppler ultrasonography. None of the patients required hospital admission.
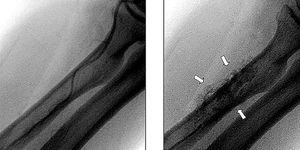
Four patients presented perforations of the radial artery and one of the humeral artery. In three of the patients there was a relationship between the attempt to advance a 0.025' hydrophilic guide through a stenotic area. In 4 patients diagnosis was done with angiography during catheterization, which showed contrast extravasation (example shown in Figure 2) while attempting to advance the guide through areas of tortuosity and radial or humeral artery spasm. As soon as the complication was identified the access route was abandoned. One patient presented increased volume of the ipsilateral forearm, distant from the puncture site (distal margin of the elbow fold) 15 min after finalizing a diagnostic procedure apparently without incident. Based on our experience with the first patient, in whom a large hematoma in the forearm appeared some minutes after identifying the contrast extravasation, the immediate treatment was the same: compression of the area and application of an external compression bandage in the ruptured area. The bandage was not removed until 4 h later, when the area was inspected and distal pulses palpated. There were no new incidents in 4 patients after a minimum follow-up of 7 days. In one patient an arteriovenous fistula was diagnosed in the perforation site during a follow-up catheterization done at 6 months due to suspicion of restenosis (Figure 3). The patient presented no symptoms related to the fistula, but a fremitus was palpated in the ipsilateral forearm. Treatment was conservative in this case.
Fig. 2. Contrast extravasation (arrows in the right panel) after a failed attempt at advancing the guide via a thin radial artery (left panel).
Fig. 3. Arteriovenous fistula as a complication of a radial perforation (angiography at 6 months). The trajectory of the vein is marked by arrows.
DISCUSSION
The radial approach offers a safer alternative to the femoral or humeral route regarding hemorrhagic complications.1-3 In line with previous studies,1-8 the present series reports a far lower frequency of complications than is commonly encountered via the femoral route and no need for surgery or blood transfusion in more than 3000 procedures.
Arteriovenous fistula manifested in very similar way in the 2 cases reported: pain, paresthesias and edema in the hand ipsilateral to the puncture. Before surgical repair we decided to attempt closure by external compression. We estimated that it would be sufficient to stop venous flow for several hours with the compression bandage, as shown in Figure 1, and to provide appropriate oral analgesia and maintain the arm at rest. Compression and rest were maintained for a long time without need for hospital admission and were effective even in a patient under anticoagulant treatment with acenocoumarol. The bandage applied was similar in the case of pseudoaneurysm, although the compression time was shorter. One of the cases of fistula occurred as a consequence of the guide used during catheterization which perforated the proximal part of the radial artery.
The most frequently encountered complication after localized hematoma was perforation of the radial or humeral artery by the guide used to advance the catheters. Although it is logical to assume that the risk of perforation is greater if a hydrophilic guide is advanced through an area of stenosis or tortuosity, in at least two cases only a Teflon-coated J-guide was used. This highlights the need to avoid force when advancing the guides or catheters if any difficulty is encountered with this approach. In most cases there were no long-term complications, although we report one patient with an arteriovenous fistula exactly at the site where the perforation had been previously encountered, probably due to this occurring at a point on the arterial wall which was very close to the trajectory of the vein.
In conclusion, even in the rare case of serious secondary hemorrhagic complications, transradial access for catheterization is easier to manage than the femoral approach, and surgical repair is the exception. The management of such complications should be understood by those beginning to use the transradial technique, and by those who are already familiar with it.
Correspondence: Dr. M. Sanmartín Fernández.
Cardiología Intervencionista. Hospital Meixoeiro.
Meixoeiro, s/n. 36200 Vigo. Pontevedra. España.
E-mail marcelo.sanmartin.fernandez@sergas.es