Patent foramen ovale (PFO) is a frequently occurring entity that is usually considered benign. However, isolated cases of platypnea-orthodeoxia syndrome (POS) through a PFO have been described. These can be highly symptomatic and difficult to identify.
Platypnea-orthodeoxia syndrome is characterized by dyspnea and oxygen desaturation that is exacerbated by the upright position. It is caused by venous blood entering systemic circulation through intracardiac or pulmonary shunting.1 For PFO to cause POS, there must have been a change in the position of the interatrial septum (IAS) to facilitate the direction of flow from the inferior vena cava towards the septum and the passage of deoxygenated blood from the right to the left atrium. This change would involve the IAS horizontalization (especially in the upright position) favored by several clinical conditions. Those described most frequently are aortic dilatation,2 chest surgery,3 pulmonary emphysema, and illnesses affecting the pericardium. Elevated right heart cavity pressure favors this shunt, but is not essential.4
In a clinical context of suspicion, diagnostic confirmation is simple. It is enough to show that microbubbles pass from the right to the left atrium in the first three cardiac cycles after opacification of the right cavities in agitated saline transthoracic echocardiography. Transesophageal echocardiography helps identify IAS defects accurately.5 Treatment usually consists of percutaneous IAS defect closure.6
We present 3 consecutive cases of POS due to intracardiac communication through a PFO diagnosed in our center in the last 2 years that illustrate the syndrome, its different clinical presentations, and the diagnostic process.
The first is that of a 40-year-old woman with a history of paraplegia due to spina bifida. The patient was admitted to an intensive care unit for septic shock of urinary origin and required intubation and mechanical ventilation due to respiratory insufficiency. After her hemodynamic situation had improved, persistent severe hypoxemia of no obvious cause was observed. Thoracic computerized tomography ruled out pulmonary thromboembolism or parenchymal disease. Hemodynamic monitoring ruled out pulmonary hypertension. The absence of any response to high concentration oxygen therapy led us to suspect the existence of a right-left shunt. Transesophageal echocardiography revealed a PFO, and right-left communication was confirmed by agitated saline transthoracic echocardiography. The patient improved after positive pressure ventilation withdrawal and extubation proceeded as planned. Percutaneous PFO closure was rejected because of the patient's good clinical tolerance, reduced mobility, and the difficulty of vascular access.
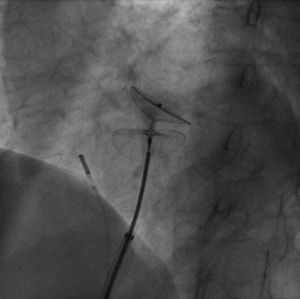
The second case is that of a 72-year-old woman with a history of arterial hypertension who, in the last 3 years, had been hospitalized on several occasions for respiratory failure. On this occasion, she was admitted for exertional dyspnea and hypoxemia. The echocardiogram showed a mildly hypertrophic left ventricle, with normal systolic function and moderate dilation of the aortic root. The computerized tomography ruled out pulmonary thromboembolism, pulmonary arteriovenous fistulas or lesions in the pulmonary parenchyma. In hospital, we observed marked oxygen desaturation in the upright position that improved when supine, which led us to suspect POS. A directed echocardiographic study was requested, and PFO and right-left communication at baseline and following Valsalva maneuver were found using agitated saline transthoracic echocardiography. A complete hemodynamic study was carried out, with intracardiac and pulmonary pressure measurements, oximetry, and angiography, and confirmed the existence of intracardiac shunt through the PFO. Following an occlusion test, which confirmed the normalization of oxygen saturation in the left heart cavities, the patient underwent percutaneous PFO closure with an Amplatzer PFO device (Figure 1) with good angiographic and subsequent echocardiographic findings. Following this, she had a significantly improved clinical condition, with normalized oxygen saturation. Improvement has continued (without needing readmission) since implantation more than 1 year ago.
Interatrial septum closure device in patient 2 prior to deployment. Deployment of the device shows the total horizontalization of the interatrial septum in the patient—causing the shunt. The horizontal position of the interatrial septum in this case is due to growth of the ascending aorta associated with arterial hypertension and age.
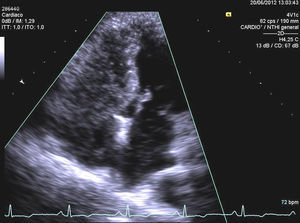
The third case is that of a 67-year-old man with a history of coronary disease in 3 vessels surgically revascularized less than 1 month previously. Both surgery and the immediate postoperative period passed without complications. One week after discharge, the patient came to the emergency department for exertional dyspnea and dizziness following exertion. He reported the absence of chest pain, orthopnea or high temperature, or other signs of heart failure. The chest X-ray was normal and the electrocardiogram showed no signs of ischemia. We found mild hypoxemia in supine position that became severe on assuming an upright position and with the slightest exertion. The patient improved slightly with oxygen therapy and was practically normal when supine. Chest computerized tomography was normal. The echocardiogram showed no abnormalities, except the IAS aneurysm. Estimated pulmonary pressure was normal. Using agitated saline transthoracic echocardiography, we found innumerable bubbles flowed from the right to the left atrium, both at baseline and following the Valsalva maneuver (Figure 2). Transesophageal echocardiography showed the existence of PFO and we diagnosed POS due to PFO triggered by changes in the anatomic disposition of the IAS following thoracotomy. Cardiac catheterization confirmed the diagnosis and a Cardia UltraSept PFO device was implanted, with excellent angiographic and echocardiographic results. After the procedure, the patient presented immediate clinical recovery, with normalization of oxygen saturation in an upright position and normal tolerance to exertion.
Echocardiographic image of both ventricles following agitated saline solution administration in peripheral vein in patient 3. Opacification of the right ventricle is shown and passage of bubbles to the left ventricle through the interatrial septum. For diagnosis, the passage of bubbles from the right to the left heart cavities should occur in the first three beats after opacification of the right heart cavities.
These 3 cases show different clinical presentations of the entity and illustrate its varied diagnostic process. The first case shows a form of subclinical presentation in a patient with a low level of physical activity in whom the syndrome was uncovered by positive-pressure mechanical ventilation. The second case shows how patients with POS and chronic respiratory insufficiency often undergo years of symptoms before receiving a diagnosis. The third case shows an acute presentation, with highly debilitating symptoms, following cardiac surgery. Note that, in terms of the diagnostic process, the first case enabled us to recognize the syndrome; the second, to confirm its presence in patients with respiratory insufficiency of unclear origin; and the third, to show how simple the diagnosis can be, given awareness of the clinical characteristics.