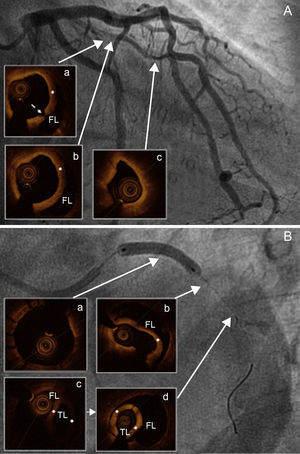
A 53-year-old man who had recently abandoned triple antihypertensive therapy was referred by his healthcare center following a first episode of angina at rest, which coincided with a significant increase in blood pressure (180/100mmHg) and was accompanied by diffuse transitory ST-segment depression. Coronary angiography showed tapering of the proximal-middle segment of the median branch, which intracoronary nitroglycerin failed to modify (Fig. 1A). As spontaneous coronary dissection (SCD) was suspected, optical coherence tomography (OCT) was used to study the vessel after unfractionated heparin (85 U/kg) was administered. The OCT confirmed focal intimal rupture (Fig. 1Aa) and revealed a double lumen proximally (Fig. 1Ab) and a subocclusive intramural hematoma more distally (Fig. 1Ac).
A: Diffuse narrowing of the lumen in the proximal-middle segment of the median branch; focal intimal rupture (a, broken arrow), with intimal flap (+) separating the false lumen (b) and the subocclusive distal intramural hematoma (c). B: Stent implant in median branch (a), complicated by distal expansion of the dissection (b), requiring a second stent after relocating the guidewire in the true lumen (c and d). FL, false lumen; TL, true lumen.
Given that the patient had experienced several episodes similar to that for which he was admitted while receiving optimal medical treatment (acetylsalicylic acid, clopidogrel, fondaparinux, beta blockers and nitroglycerin), as well as the elevated troponin T observed (11 ng/mL), and his good median branch caliber, the treatment of choice was percutaneous revascularization with a direct drug-eluting stent (3×38mm at 14 atm), which would completely cover the hematoma and intimal rupture (Fig. 1B). Using OCT, we confirmed the adequate seal and stent placement (Fig. 1Ba), although OCT also disclosed distal progression of the dissection, causing substantial obstruction of the vessel (Fig. 1Bb) and the distal deployment of our guidewire in the false lumen (Fig. 1Bc). After relocating the guidewire in the true lumen (Fig. 1Bd), a second drug-eluting stent was overlapped distally.
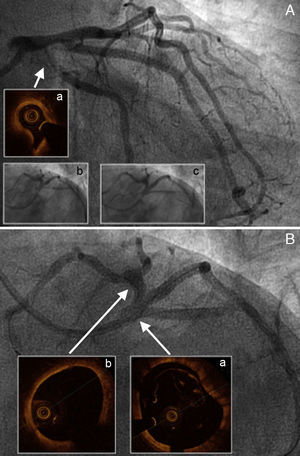
Subsequent angiography revealed proximal progression of the hematoma causing severe lumen reduction in the median branch ostium and circumflex artery (Figs. 2A and Aa), which required 2 drug-eluting stent implants (Figs. 2Ab and Ac).
A: Affected medial branch ostium and circumflex artery, with much-diminished circumflex artery lumen caused by compression from the hematoma (a); stent implants at both levels (b and c). B: Final angiogram showing neither compromised lumen and flow in the left coronary artery nor images of dissection in the left main coronary artery (a) or left anterior descending artery (b).
We finally confirmed satisfactory angiographic results for the intervention (Fig. 2B) when OCT visualized adequate stent placement at the ostial level–which did not protrude into the left main coronary artery–and showed that the dissection had not progressed this far (Fig. 2Ba) or to the left anterior descending coronary artery (Fig. 2Bb). The patient was discharged with no new complications.
From our point of view, the patient and his clinical course raise several interesting issues. Firstly, although SCD has typically been described in young women with no cardiovascular risk factors we should not forget that it also affects middle-aged men (<20%-30% of patients).1,2 The (unclear) pathophysiology of SCD has been attributed to intramural hematoma formation originating in inflammatory atherosclerotic processes, rupture of vasa vasorum, or vascular changes arising during pregnancy.2 However, it is highly likely that in our patient–in the absence of other cardiovascular risk factors, obstructive atherosclerotic lesions, family history or connective tissue disease–the determining factor would have been parietal stress caused by poor blood pressure control.
Secondly, this patient exemplifies the difficulties of percutaneous treatment of SCD. As we have seen, it is not without complications due to frequent proximal and distal expansion of the hematoma, entailing the risk of having to implant more stents than intended. Given that the prognosis is usually favorable, medical treatment is recommended except in patients showing clinical and/or hemodynamic instability, large caliber vessels or significantly reduced distal flow.2,3
Moreover, this case emphasizes the value of OCT in the diagnosis and treatment of SCD. Prior to the routine use of coronary angiography, the real incidence of SCD was underestimated2 and, without the help of intracoronary diagnostic techniques (OCT or intravascular echocardiography), this will continue.1 While the typical angiographic image of SCD is that of a flap with 2 or more lumen, often only a narrowing of the lumen can be observed. This can be misinterpreted as an atherosclerotic lesion, especially if the clinical presentation gives no cause to suspect SCD, leading to errors in patient management. Although the OCT does not always manage to identify an intimal rupture, it does detect the intimal flap and thus enables visualization of the 2 lumen; as they are sometimes occupied by thrombus,1 this could justify the absence of double lumen images in angiographic studies.
Finally, we would stress that these techniques are essential in percutaneous treatment. As well as determining the extension of SCD, which aids the choice of the appropriate length and diameter of the stent to be deployed, OCT enables us to confirm correct placement of the angioplasty guidewire in the true lumen since, as we have said, it is not unusual for it to advance through the dissection itself. If complications occur, OCT is essential for their early identification and adequate resolution, and to determine the correct final result in terms of sealing the dissection and the expansion and placement of the stent.
FundingDr. Juan Ruiz-García would like to thank the Spanish Society of Cardiology for financial support received through the Hemodynamics and Interventional Cardiology section's 2011 Post-Residency Research Training Grant.
.