Over the last 20 years, cardiac surgery has evolved toward less invasive procedures, with the aim of reducing the surgical insult to the body and achieving early patient recovery. Currently, the standard surgical approach for the treatment of mitral disease remains full median sternotomy; however, minimally invasive techniques have become established as a safe and effective alternative used routinely in specialized centers, associated with excellent short-term and long-term outcomes and lower morbidity.1,2 The right anterior minithoracotomy is the most common minimally invasive approach for mitral valve surgery. This technique allows treatment of the tricuspid valve, atrial defects, and atrial fibrillation at the same time.3
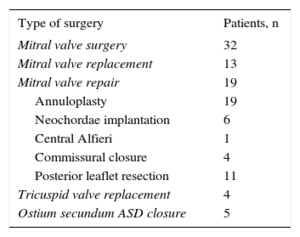
We present our initial experience and results with this minimally invasive approach. Between January 2012 and December 2015, 40 patients underwent intervention in our hospital. There was a predominance of men (62.5%), and the mean age was 58.5 years (range, 22-81 years). All patients had a right anterior minithoracotomy (incisions of 6 cm to 8 cm) plus 3 accessory ports < 5mm, according to the surgical requirements (for Chitwood clamp, atrial retractor, and vent). All patients were connected to extracorporeal circulation by peripheral cannulation of the femoral vessels (artery and vein): a single 2-stage venous catheter was positioned in the superior vena cava in the first 12 patients, with subsequent cannulation of the right jugular vein in the remaining patients. A CO2 laser was used in all operations. Beating heart surgery was performed, without ischemia in 4 patients, and with moderate hypothermia in 8 patients who were in ventricular fibrillation. The remaining patients proceeded to transthoracic aortic cross-clamping with a Chitwood clamp, with antegrade cardioplegia through the aortic root via the ministernotomy. The mean time on extracorporeal circulation was 140±38minutes and the mean ischemia time was 98±27minutes. The Table shows the types of operation performed in these patients; notably, around half the operations were mitral valve repairs.
Type of Surgery Performed Via Right Anterior Minithoracotomy
| Type of surgery | Patients, n |
|---|---|
| Mitral valve surgery | 32 |
| Mitral valve replacement | 13 |
| Mitral valve repair | 19 |
| Annuloplasty | 19 |
| Neochordae implantation | 6 |
| Central Alfieri | 1 |
| Commissural closure | 4 |
| Posterior leaflet resection | 11 |
| Tricuspid valve replacement | 4 |
| Ostium secundum ASD closure | 5 |
ASD, atrial septal defect.
In our series, there have been no recorded deaths, either in-hospital or in the longer-term. At follow-up, all the repaired mitral valves were competent and free from regurgitation and reoperation. The most significant postoperative complications were as follows: 1 case of air embolism with mild transient neurological deficit (delirium and psychomotor agitation) with complete recovery at the time of hospital discharge; 1 case of failed mitral valve repair, with reintervention via minithoracotomy during the same admission to perform a new valvular repair; 1 patient with prolonged mechanical ventilation due to adult respiratory distress syndrome with complete recovery at the time of hospital discharge; and 1 conversion to full median sternotomy due to bleeding after the procedure was finished, caused by damage to the pulmonary artery after release of the aortic clamp. The remaining patients’ hospital stays were < 5 days, with no postoperative pain and recovery of normal activities in 2 weeks (Figure). Therefore, regarding morbidity and mortality, the results of our series are comparable to those of other published studies.1,4
According to the literature, compared with those with conventional treatments, patients who undergo surgery with minimally invasive approaches have fewer arrhythmias, less bleeding and need for transfusion, shorter stays in intensive care and in hospital, earlier extubation, less postoperative pain, and an earlier recovery of functional status and daily activities, with greater patient satisfaction and a better aesthetic result.1,2 Despite the lower morbidity, these techniques are not performed routinely in all hospitals, as they are more technically demanding for the surgeons, have longer operating times (ischemia time and extracorporeal circulation time), and are accompanied by the corresponding learning curves and need for dedicated, costly materials.3,4 In the future development of cardiac surgery, minimally invasive surgery has an essential role in responding to the demands of both patients and cardiologists; it is comparable to interventional procedures5 and an excellent technique for the surgical approach in patients with previous cardiac surgery.1,2,6 Therefore, in various hospitals, minimally invasive surgery appears to be an increasingly popular technique as an alternative to conventional surgery. Prospective, randomized studies are needed to allow a better evaluation of the clinical outcomes and cost-efficiency of this technique.