To the Editor,
Traumatic rupture of the thoracic aorta (TAR) is associated with high mortality. It is considered the second cause of death in patients with multiple trauma, only exceeded by intracranial hemorrhage. Above all, TAR is caused by deceleration in traffic accidents. It is estimated that less than 25% of patients with intracranial hemorrhage reach hospital alive and that 50% of those who do will die within 24h.1 In 90%, rupture occurs at the aortic isthmus; in the remaining 10%, rupture is located elsewhere, eg, at the aortic root or ascending aorta. Unless treated, mortality is 85% to 90%.2 Lesions are classified as type I (intimal defect), type II (intramural hematoma), type III (pseudoaneurysm) and type IV (rupture with active bleeding).3 A “wait-and-see” approach is recommended for type I lesions, whereas the other types require emergent treatment within 24h.
Conventional open surgery (COS) requires left lateral thoracotomy, single-lung ventilation and extracorporeal circulation; early mortality is 10% to 28% and paraplegia ≤16%.3 In recent years, developments in thoracic endovascular repair (TEVR) have been spectacular and it now offers long-lasting aortic repair through a minimally invasive technique, mortality has fallen by half and paraplegia is down to 2%, making TEVR the treatment of choice for this pathology.
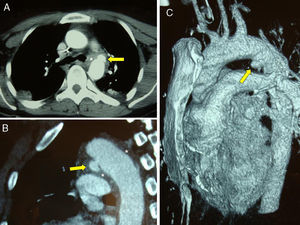
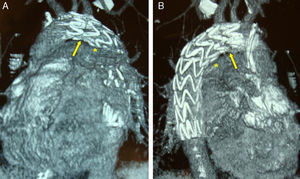
We present the case of a 28-year-old patient with multiple trauma who was admitted to our center following a traffic accident. The patient underwent thoracoabdominal computed tomographic angiography (CTA) and numerous X-rays were taken. Images showed displaced fractures of femora, radii, ulnas, and pelvis; bladder rupture; and aortic pseudoaneurysm (type III lesion, 12×8mm) at the level of the isthmus, 10mm distal from the left subclavian artery (LSA) outlet (Figure 1). The patient was stabilized, sedated, and intubated. Once absence of active bleeding had been confirmed, beta blockers were administered to maintain blood pressure at <120/80mmHg. We decided to undertake emergent TEVR with a 26×26×150mm Medtronic Valiant covered stent graft (Medtronic; Santa Monica, California, USA) using left common femoral artery access, occluding 50% of the LSA ostium, under general anesthesia to exclude the pseudoaneurysm from the systemic circulation. Final results were good with no complications. At 1 week, a follow-up CTA demonstrated absence of endoleaks and correct stent deployment with complete exclusion of the pseudoaneurysm (Figure 2). At 3 months follow-up, the patient was asymptomatic.
Figure 1. Preoperative computed tomographic angiography. Pseudoaneurysm (arrow) with periaortic hematoma (asterisk). A, axial slice; B, sagittal slice; C, 3D reconstruction.
Figure 2. Follow-up computed tomographic angiography at 1 week. Base of covered stent (arrow), covering 50% of the left subclavian artery. The asterisk indicates the previous pseudoaneurysm. A, left lateral view; B, right lateral view.
TAR is a severe lesion and management is difficult due to the need for aortic repair in addition to the range of severe lesions these patients usually present. Tang et al.4 recently compared TEVR with COS in a review of 33 publications and 699 patients. They found lower incidence of mortality (7.6% vs 15.2%), paraplegia (0.3% vs 5.6%) and stroke (0.8% vs 5.3%) in TEVR. Their data are confirmed by other experienced centers.5.
Because of concern about using TEVR in TAR patients, who are generally young and have substantial life expectancy, and because the long-term durability of current devices is unknown, the American Society for Vascular Surgery has recently published clinical practice guidelines.6 They reviewed 139 studies with 7768 patients and determined TEVR is preferable to COS, independently of age. They also recommended undertaking TEVR within 24h of TAR diagnosis, using conservative management in uncomplicated type I lesions only, not systematically performing LSA revascularization in cases of occlusion, oversizing the device by 10% maximum, surgically exposing the femoral arteries, using general anesthesia, and not systematically using spinal fluid drainage (Class IIa indication, Level of Evidence C in all cases).
In these patients, long-term follow-up with imaging techniques–especially ACT–is vital. Although the risk of radiation must be considered, in some cases serial X-rays or magnetic resonance imaging can be used (with nitinol devices only) during follow-up.
These studies all support the view that TEVR should be the technique of choice in patients with TAR–even young ones–because it is associated with lower morbidity and mortality than COS, assuming the aortic anatomy permits it and ≥10mm proximal anchorage exists. This means complete or partial LSA ostium occlusion is often needed. Revascularization should be avoided unless the patient has an incomplete Circle of Willis or subsequent complications occur.
Finally, more long-term studies are needed to determine actual device durability, the need for subsequent endovascular interventions, and the appearance of late complications, although we cannot forget that these patients have a long life expectancy and their exposure to radiation should be kept to a minimum.
.
Corresponding author: erodriguezcaulo@hotmail.com