Noncompaction cardiomyopathy (NCC) is thought to arise due to an arrest of the normal myocardial compaction process during intrauterine life.1 Clinical manifestations include heart failure, embolic events, and arrhythmias.2 Its prognosis varies considerably between studies and remains largely unknown.
Our aim was to better define the outcomes of symptomatic adult patients (defined as those > 18 years old, presenting with heart failure, atrial or ventricular arrhythmias, or embolic events) with NCC and compare them with those of a contemporary cohort of patients with idiopathic dilated cardiomyopathy (IDC).
This retrospective study included all consecutive patients who fulfilled echocardiographic criteria of NCC,3 managed at 2 tertiary centers from 2001 to 2015. As a comparison group, we included all consecutive symptomatic patients with IDC managed at the Heart Failure Program of one of the participating centers from 2008 to 2015. We collected adverse events during follow-up, defined as sustained ventricular arrhythmias, cardioembolic events, cardiovascular death, or heart transplant. The study was approved by the clinical research ethics committees of both centers. Comparative analysis between the groups were performed with the Mann-Whitney test for continuous variables and the chi-square test for categorical variables. Survival analyses were performed with Kaplan-Meier curves and differences were tested using the log-rank test. To evaluate whether NCC predicted outcomes compared with IDC, we performed a backward step multivariate Cox proportional hazard analysis.
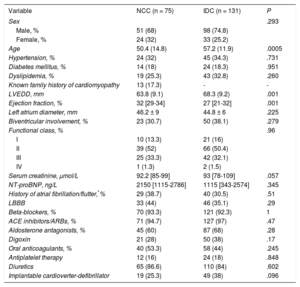
The Table shows the patients’ baseline characteristics and treatment. Seventy-five patients with NCC fulfilled the inclusion criteria. In 65 (86.7%) patients, heart failure was the index complaint, whereas 9 (12%) had arrhythmias (6 atrial in origin and 3 ventricular tachycardia [2 sustained VT with hemodynamic stability and 1 with frequent runs of symptomatic nonsustained VT]) and 1 (1.3%) presented with an embolic event (stroke); 17% of the patients with NCC had a known family history of cardiomyopathy at diagnosis (but had not previously undergone family screening).
Baseline Characteristics
| Variable | NCC (n = 75) | IDC (n = 131) | P |
|---|---|---|---|
| Sex | .293 | ||
| Male, % | 51 (68) | 98 (74.8) | |
| Female, % | 24 (32) | 33 (25.2) | |
| Age | 50.4 (14.8) | 57.2 (11.9) | .0005 |
| Hypertension, % | 24 (32) | 45 (34.3) | .731 |
| Diabetes mellitus, % | 14 (18) | 24 (18.3) | .951 |
| Dyslipidemia, % | 19 (25.3) | 43 (32.8) | .260 |
| Known family history of cardiomyopathy | 13 (17.3) | - | - |
| LVEDD, mm | 63.8 (9.1) | 68.3 (9.2) | .001 |
| Ejection fraction, % | 32 [29-34] | 27 [21-32] | .001 |
| Left atrium diameter, mm | 46.2 ± 9 | 44.8 ± 6 | .225 |
| Biventricular involvement, % | 23 (30.7) | 50 (38.1) | .279 |
| Functional class, % | .96 | ||
| I | 10 (13.3) | 21 (16) | |
| II | 39 (52) | 66 (50.4) | |
| III | 25 (33.3) | 42 (32.1) | |
| IV | 1 (1.3) | 2 (1.5) | |
| Serum creatinine, μmol/L | 92.2 [85-99] | 93 [78-109] | .057 |
| NT-proBNP, ng/L | 2150 [1115-2786] | 1115 [343-2574] | .345 |
| History of atrial fibrillation/flutter,*% | 29 (38.7) | 40 (30.5) | .51 |
| LBBB | 33 (44) | 46 (35.1) | .29 |
| Beta-blockers, % | 70 (93.3) | 121 (92.3) | 1 |
| ACE inhibitors/ARBs, % | 71 (94.7) | 127 (97) | .47 |
| Aldosterone antagonists, % | 45 (60) | 87 (68) | .28 |
| Digoxin | 21 (28) | 50 (38) | .17 |
| Oral anticoagulants, % | 40 (53.3) | 58 (44) | .245 |
| Antiplatelet therapy | 12 (16) | 24 (18) | .848 |
| Diuretics | 65 (86.6) | 110 (84) | .602 |
| Implantable cardioverter-defibrillator | 19 (25.3) | 49 (38) | .096 |
ACE, angiotensin-converting enzyme; ARBs, angiotensin-receptor blockers; LBBB, left bundle branch block; LVEDD, left ventricle end-diastolic diameter; NCC, noncompaction cardiomyopathy; NT-proBNP, N-terminal pro-B-type natriuretic peptide.
The data are expressed as No. (%), mean ± standard deviation, or median [interquartile range].
Patients with IDC were older and showed larger left ventricular end-diastolic diameters, as well as lower ejection fraction.
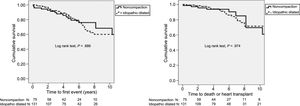
The patients were followed up for a median of 5 (2.4-6.7) years. During follow-up, 14 (18.7%) patients in the NCC group had a first adverse event (5 ventricular arrhythmias, 3 cardiovascular deaths, 4 cerebrovascular embolic events, and 2 heart transplants), whereas 35 (26.7%) patients had a first adverse event in the IDC group (13 ventricular arrhythmias, 12 cardiovascular deaths, 3 cerebrovascular embolic events, and 7 heart transplants). None of the patients with cerebrovascular events were under anticoagulant treatment prior to the event.
In the NCC group, 19 (25.3%) patients underwent an ICD placement, 12 as primary prevention and 7 as secondary prevention. In the IDC group, 48 patients (36.6%) underwent an ICD placement, 24 as primary prevention and 24 as secondary prevention. No statistically significant differences were found in terms of the ICD implantation rate between groups. Only patients in whom the indication was secondary prevention showed ICD therapies during follow-up.
The Figure shows the Kaplan-Meier survival curves free from a first event and free from cardiovascular death or heart transplant in both groups. Having an NCC did not predict a different outcome free from a first event compared with IDC (HR, 1.01; 95%CI, 0.49-2.10; P = .98) after multivariate adjustment for age, left ventricular end-diastolic diameter, ejection fraction, and serum creatinine.
Our main finding is that symptomatic adult patients with NCC had a similar incidence of adverse events and survival compared with patients with IDC. The annual incidence of thromboembolic events was 1.06 percent per year in the NCC group and 0.62 percent per year in the IDC group. Interestingly, both groups showed a high incidence of anticoagulation therapy, even in sinus rhythm, but a diagnosis of NCC was not an indication for the use of anticoagulants. The low rate of thromboembolic events was probably related to this high incidence, and anticoagulation with a tight control of the therapeutic range may benefit patients with left ventricular dysfunction in sinus rhythm.4 The prevalence of ventricular arrhythmias and rates of ICD implants did not differ significantly between the 2 groups.
This study has several limitations. First, this is a retrospective study with limited statistical power. A major limitation is that only echocardiography was used as a method of diagnosing patients with NCC and this could overestimate the real number of patients, given the limitations of the echocardiographic diagnostic criteria.5 Even though 50 patients (66.6%) with echocardiographic NCC underwent cardiac magnetic resonance imaging to complete the study, the use of this technique was uneven across the cohort. Of note, NCC was confirmed in all the patients who underwent magnetic resonance imaging. Importantly, only a minority of our patients underwent genetic testing. Finally, the presence of neuromuscular disorders was not evaluated and all patients came from and were followed up at heart failure units; this may have created a possible selection bias which could influence the observed outcomes.
In conclusion, our study shows a nonsignificant effect of NCC on mortality compared with IDC in symptomatic adult patients being followed up at specialized heart failure units.