Lemierre syndrome, also known as postanginal sepsis, is a very rare complication of acute tonsillitis, as yet undescribed in adult patients with Fontan circulation. It is usually caused by the anaerobic bacteria Fusobacterium necrophorum, part of the normal flora. Although the term Lemierre syndrome has been applied to different clinical situations,1,2 it is characterized by thrombophlebitis of the internal jugular vein and distal septic emboli following acute tonsillitis.
We present the case of a teenage boy with complex congenital heart disease with Fontan circulation who developed multiorgan failure and multiple metastatic septic emboli.
This was an 18-year old patient, with no history of substance abuse and a medical history of complex congenital heart disease: dextrocardia with situs solitus, with a double-inlet, double-outlet right ventricle, transposition of the great vessels, subvalvular pulmonary stenosis, and an ostium secundum interatrial communication. He had undergone a palliative bidirectional Glenn procedure and subsequent total cavopulmonary connection with fenestration.
The patient presented with a 3-day history of somnolence, odynophagia, and fever. He was referred from another center with suspected endocarditis. On examination, he was febrile (41°C), pale, and peripherally underperfused. He had a right parasternal systolic murmur, lungs were normal on auscultation (pO2 52 mmHg on 100% oxygen), heart rate was 140 bpm, and blood pressure was 85/50 mmHg. Oropharynx examination showed good dentition and pharyngeal erythema. There was no lymphadenopathy. Blood tests showed leukocytosis (45 700 cells/mL; 92% neutrophils), thrombocytopenia (54 000 cells/mL), prolonged clotting times, glucose 50mg/dL, normal creatinine kinase, and elevated AST, ALT, bilirubin, procalcitonin, lactic acid, and creatinine.
Echocardiography showed a single ventricle with right ventricular morphology and a double inlet, severe ventricular dysfunction, moderate left atrioventricular (systemic) regurgitation, redundant valve leaflets with excess tissue, no images compatible with vegetations, slow-flow Fontan circulation, right-to-left systodiastolic flow through the fenestration, and the superior vena cava draining to the right pulmonary artery (Glenn) with no flow acceleration.
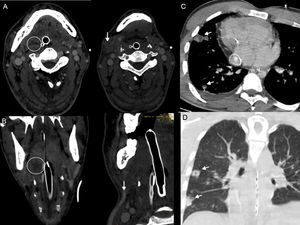
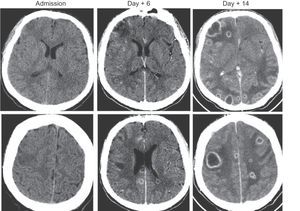
Computed tomography of the head, neck and chest showed a right peritonsillar fluid collection, an intraluminal filling defect at the level of the right facial and external jugular veins, hypodense cerebral lesions in both hemispheres (which on follow-up scans showed contrast uptake with subcortical enhancement), no evidence of intracranial venous sinus thrombosis, and multiple cavitating right-sided pulmonary nodules (Figure 1 and Figure 2).
A: computed tomography of the neck, axial view. B: coronal multiplanar reconstruction: right peritonsillar collection (circle) and thrombosis of right facial vein (arrow). C: late-phase computed tomography of the chest; Gore-Tex graft (Fontan) (asterisk). D: coronal view, dextrocardia; multiple cavitating pulmonary nodules (arrows).
The tonsillar collection was incised and drained. Blood cultures were positive for F. necrophorum.
The patient developed severe respiratory failure secondary to primary lung injury and an increased right-to-left shunt, distributive and cardiogenic shock, acute renal and hepatic failure, and anemia. He required invasive ventilatory and inotropic support, continuous renal replacement therapy, and hyperthermia control using surface techniques. His hemodynamic, respiratory, and neurological status improved, and he was sent to his home country conscious and with no focal neurology.
Lemierre syndrome is a rare but not exceptional condition that can complicate the clinical course of an oropharyngeal infection even when treated appropriately.
The signs and symptoms of the disease relate closely to its pathogenesis, which has several stages: primary infection with acute pharyngotonsillitis, invasion of the parapharyngeal space, and metastatic infection.
The most common site of septic embolization are the lungs, but other areas can be affected. In this patient, the presence of embolic lesions predominantly in the right lung was probably due to preferential flow toward the right lung (as shown on magnetic resonance imaging), despite the superior cavopulmonary connection being bidirectional.
Less information is available on neurological involvement in this disease. Isolated cases have been described of meningitis due to F. necrophorum or sinus thrombosis (sigmoid or cavernous) from retrograde propagation of thrombophlebitis in the internal jugular vein. In this patient, the cerebral infarcts that developed into multiple abscesses were probably caused by paradoxical septic emboli due to the presence of a right-to-left cardiac shunt through the Fontan fenestration.
Diagnosis of Lemierre syndrome can be difficult on account of the unusual clinical picture, although it should be suspected in any case of severe sepsis with a recent history of oropharyngeal infection.
Early and prolonged antibiotic treatment, anticoagulation, and sometimes surgical excision of the jugular veins have improved survival. In this patient, anticoagulation was contraindicated by the cerebral lesions and severe thrombocytopenia. Follow-up echocardiography scans showed repermeation of the jugular and facial veins and improved flow in the right cavopulmonary communication and Fontan circulation.
Fontan circulation, the definitive palliative treatment for patients with complex congenital heart disease with a functional univentricular heart, complicates clinical, hemodynamic, and respiratory treatment,3 especially for patients with a single ventricle with right ventricular morphology. The absence of a subpulmonary ventricle and the invasive mechanical ventilatory support with loss of negative inspiratory pressure make it difficult to generate a pressure gradient in the pulmonary circulation. This compromises the efficiency of the Fontan circulation and increases the right-to-left shunt in cases of a fenestrated Fontan. Any situation that affects this pressure gradient must be avoided: this includes increases in intrathoracic pressure, excess fluid balance, and increased end-diastolic left ventricular pressure.