The current evidence indicates the default use of a radial approach for percutaneous coronary procedures because it reduces the risk of severe complications and improves patient comfort. The success of transradial procedures and their potential benefits can be undermined by loops and tortuosities in the axis formed by the subclavian artery, innominate artery, and aortic arch.1,2 The difficulties posed by these loops and tortuosities are generally handled in a stepwise manner.3 Most cases are resolved using conventional maneuvers, such as by instructing the patient to take a deep breath or via the use of catheters with a wider diameter. Other maneuvers that can be considered are the use of more rigid guidewires or longer sheaths up to 80cm in length or a change of vascular access. Here, we propose a novel technique for the treatment of aortosubclavian tortuosities and loops that cannot be corrected using conventional maneuvers: the parallel wire technique.
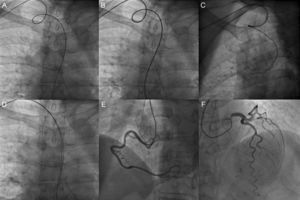
We begin with a general description of the technique. The maneuver is based on the advancement of an additional 0.035-inch hydrophilic diagnostic guidewire (Radifocus Stiff, Terumo) from the radial artery to the aorta in parallel with the catheter and initial diagnostic guidewire. Once both guidewires are positioned in the aorta, the catheter is advanced on one of them; this guidewire is then removed. The companion guidewire remains in place in the aorta parallel to the catheter and the loop or tortuosity is straightened, which facilitates catheter manipulation, stability, and support. As precautions, the guidewire should be supported on the aortic valve with its distal end beyond the coronary ostia. In addition, when catheter exchange is required, the position of the guidewire should be actively maintained to avoid its dislodgement. A representative example illustrating application of the technique can be seen in Figure.
Coronary angiography via a right radial approach showing a loop in the axis of the subclavian-innominate arteries (A) that could not be corrected using simple maneuvers (B). Partial withdrawal of the guidewire (Radifocus Stiff, Terumo) resulted in catheter retraction (C), which impeded stable exploration of the coronary arteries. Parallel advancement of an additional guidewire (Radifocus Stiff, Terumo) to the aortic root corrected the loop (D) and allowed completion of the left and right coronary angiography without other incidents (E, F).
As shown in the Table, the parallel wire technique was used in a consecutive series of 10 patients with loops and tortuosities in the aortosubclavian axis that were not amenable to correction via conventional maneuvers. These patients were derived from a 3-year period. In this time, 5213 coronary procedures were performed, 97% via vascular access from an upper extremity. Two of these patients had previously undergone procedures during which the vascular access had to be changed due to the presence of these loops or tortuosities. In all patients, the initial sheath was exchanged for a 7-Fr femoral sheath over the initial diagnostic guidewire. In no case did the companion guidewire interfere with catheter manipulation. There were no technique-related complications. The position of the guidewire was always maintained during the catheter exchange. In 1 patient, 2 parallel guidewires were required to keep the loop straight.
General Description of the Series
| Patient | Age, y | Sex | CVRFs | Initial approach | Difficulty | No. of guidewires | Procedure | Catheter | Duration, min | RP | Comp | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Type | Ca++ | Diagnostic | Guidewire | |||||||||||
| 1 | 73 | M | HT, DL | 5 Fr, RR | CL | No | 2 | Diagnostic | Elective | 5-Fr Blk | - | 15 | Yes | No |
| 2 | 75 | M | HT | 6 Fr, RR | CL | No | 2 | Therapeutic | Urgent | - | 5-Fr MAC4 | 62 | Unknown | No |
| 3 | 64 | M | HT, Ob, ExS | 6 Fr, RR | SL | Yes | 2 | Diagnostic | Elective | 5-Fr Blk | - | 41 | Unknown | No |
| 4 | 80 | M | T2DM, DL | 6 Fr, RR | CT | Yes | 2 | Therapeutic | Elective | - | 5-Fr EBU3.5 | 26 | Yes | No |
| 5 | 75 | M | HT, ExS | 5 Fr, RR | ST | No | 2 | Diagnostic | Elective | 5-Fr Blk | - | 107 | Yes | No |
| 6 | 70 | W | HT, DL | 5 Fr, RR | CL | No | 2 | Diagnostic | Elective | 5-Fr Blk | - | 44 | Yes | No |
| 7 | 85 | M | HT | 6 Fr, RR | CL | Yes | 2 | Therapeutic | Urgent | - | 5-Fr MAC3/EBU 3.5 | 43 | Unknown | No |
| 8 | 83 | M | HT, DL | 6 Fr, RR | CT | Yes | 2 | Therapeutic | Urgent | - | 5-Fr AL2 | 120 | Yes | No |
| 9 | 80 | W | T2DM, DL | 5 Fr, RR | CL | Yes | 3 | Diagnostic | Elective | 4-Fr JL 3.5 | - | 63 | No | No |
| 10 | 72 | M | ExS | 6 Fr, RR | ST | Yes | 2 | Therapeutic | Urgent | - | 5-Fr AL2 | 60 | Yes | No |
AL, Amplatz left curve catheter; Blk, multipurpose BLK diagnostic curve catheter; Ca++, vessel calcification visible on fluoroscopy; CL, complex loop; CT, complex tortuosity; CVRF, cardiovascular risk factor; DL, dyslipidemia; EBU, Extra Back Up curve guidewire; ExS, exsmoker; HT, hypertension; JL, Judkins Left diagnostic curve catheter; M, man; MAC, MAC curve guidewire; Ob, obesity; RP, presence of radial pulse in follow-up; RR, right radial artery; SL, simple loop; ST, simple tortuosity; T2DM, type 2 diabetes mellitus; W, woman.
CL, angulation > 360° small diameter turn; SL, angulation > 360° large diameter turn; CT, angulation > 90° ≥ evident Ca++ ± complex morphology; ST, angulation < 90° ≥ evident Ca++.
Duration: procedure duration recorded automatically by a polygraph from the entry of administrative data to case closure. Technique-related complications could include pain requiring rescue analgesia, radial spasm, thrombosis, embolism, or dissection due to the companion guidewire. In all patients, an intra-arterial bolus of 3000 IU of sodium heparin and nitroglycerin was introduced at procedure initiation.
The technique has some limitations. The use of 7-Fr sheaths might be difficult in some patients. The mean diameter of the radial artery is small, which is why it is also susceptible to atheromatous disease. Thus, the availability of hydrophilic sheaths with a 6-Fr external diameter and a 7-Fr internal lumen (Glidesheath Slender, Terumo) might be useful due to their lower external diameter. Finally, the maximum diameter of the catheters used was 5 Fr because, with the parallel guidewire in position, the sheaths did not permit the use of catheters with a larger diameter. When techniques requiring catheters of 6 Fr or higher are considered necessary, a change in vascular access is recommended.
In conclusion, our series suggests that the parallel wire technique is safe, simple, and reproducible. It improves catheter manipulation, support, and stability. The procedure, although novel, can be added to the repertoire of strategies available for tortuosities and loops in the axis of the subclavian and innominate arteries and the aortic arch that cannot be corrected using conventional maneuvers. Our technique extends the benefits of radial access to patients with these types of complex vasculature, who are frequently affected by procedural failure.