Keywords
INTRODUCTION
Kawasaki Disease (KD) is an acute febrile childhood disease1 capable of damaging the coronary arteries and causing aneurysms, which can then become complicated with thrombosis or coronary obstruction, leading to myocardial ischemia.2
METHODS
Between October 1988 and April 2004, we assessed 150 children with KD. The mean age was 44.8 months (range, 3-114); 56 were girls and 94 were boys. Patients with "typical" American Heart Association (AHA)3 criteria were included: prolonged fever (≥5 days) plus 4 of the following criteria: a) changes in extremities, b) polymorphic exanthem, c) bilateral conjunctivitis without exudate, d) changes in oral cavity, and e) cervical lymphadenopathy. "Atypical or incomplete" cases with fever ≥5 days and fewer than 4 criteria, but with coronary artery complications on echocardiography, were also included.4
Laboratory tests, including complete blood counts, erythrocyte sedimentation rate (ESR), and platelet count, were performed. The cardiac complications of KD were assessed by color Doppler echocardiography from the fifth day, except in three patients due to a late echocardiographic finding, a retrospective diagnosis of KD in one child with angina, and a postmortem diagnosis in 1 infant with prolonged fever. The presence and degree of valvular, myocardial, and pericardial compromise were determined, as well as the presence and type of coronary lesions, which were classified as follows:
1. Diffuse ectasia or dilation (diameter greater than that expected for the body surface area).5
2. Coronary aneurysm (segmental dilation >1.5 times the adjacent segment)6; it was also indicated whether the aneurysm was single or multiple, small and/or medium-sized (up to 8 mm) or giant (over 8 mm).7
3. Coronary stenosis.
Echocardiography was repeated in 4-6 weeks and at 1 year from the onset of symptoms in patients with no heart disease, every 6 months in those who had small to moderately sized aneurysms, and every 1-3 months in children with giant aneurysms. From 5 years of age, the patients were evaluated by a yearly stress test. Patients with residual moderate or giant coronary aneurysms also underwent perfusion myocardial testing (single photon emission computed tomography [SPECT]) at rest and with pharmacologic challenge every two years after 10 years of age.8 Coronary angiography was indicated in a child who consulted for angina and experienced an acute myocardial infarction (AMI).
The comparison of quantitative variables between patients who developed an aneurysm and those who did not was done by one-way analysis of variance in the case of parametric distributions and the Mann-Whitney/Wilcoxon test for 2 samples in the case of nonparametric distributions. The association between the qualitative characteristics and the development of aneurysms was assessed by a χ² test using the Yates correction or by Fisher's exact test.
RESULTS
A total of 27 patients (18%) experienced cardiac complications.
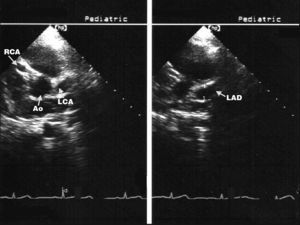
Mitral regurgitation was mild, transient, and uncommon (3.7%). Three male patients who developed giant coronary aneurysms presented pancarditis (Figure). There were no cases of aortic valvulitis.
Figure. Echocardiographic image (short axis of large vessels) showing coronary aneurysms. Ao indicates aorta; LAD, left anterior descending artery; LCA, left coronary artery; RCA, right coronary artery.
All had coronary lesions, which were classified as follows:
- Group 1: transient dilation (ectasia) in 11 patients.
- Group 2: single aneurysm of small or moderate size in 9 patients (group 2a) and multiple aneurysms of small or moderate size in 3 patients (group 2b).
- Group 3: giant coronary aneurysms in 3 patients.
- Group 4: coronary stenosis in 1 patient (Table 1).
Follow-up was from 1 to 16 years (mean, 8.5 years). In total, 147 children received treatment following the diagnosis: oral acetylsalicylic acid (ASA) (80 mg/kg/day) and intravenous gamma globulin (400 mg/kg for 4 consecutive days until 1992 and later 2 g/kg as a single dose). In 43 patients, treatment was administered after 8 or more days of fever; 13 patients already had coronary aneurysms. On the third day of apyrexia, ASA was reduced to 3-5 mg/kg/day, maintaining it until the sixth week from the onset of symptoms in patients with no aneurysms or until the aneurysms were no longer visualized on echocardiography. No new lesions occurred after the administration of gamma globulin.
We compared the clinical and laboratory data of the patients without (group A) and with (group B) coronary compromise.
In group B, coronary lesions predominated in children under 2 years and in school-aged children (5-10 years). Boys were affected more often in both groups, but only boys had serious coronary lesions. In group B, 44% presented typical KD and 56%, incomplete forms of the disease (without statistical significance).
Group B had more prolonged fever than group A (8 vs 6 days; P<.05) and the average ESR was 70 mm in group B and 48 mm in group A (P<.05) (Table 2).
There were no differences in the number of leukocytes or platelets.
In the patients with coronary ectasia, diameters returned to normal within the first 45 days of KD; the aneurysm regressed in 100% of group 2a patients within the first 3 years of follow-up and persisted in 66% of group 2b patients, although without complications during clinical follow-up and with stress and/or myocardial perfusion testing.
Among the 4 patients with giant aneurysms, 1 died undiagnosed; another had an AMI (which required coronary bypass surgery) and the other 2 were asymptomatic, with no ischemia detectable by noninvasive tests (3 and 15 years of follow-up).
DISCUSSION
Kawasaki disease is an acute vasculitis of unknown origin that occurs in childhood1 and is predominantly observed among boys under 5 years of age.9 Our patients under 27 months, but also those of school age (5-10 years), had a higher incidence of cardiac complications.10
Kawasaki disease can affect the valvular endocardium, myocardium, and/or pericardium.7 In our series, mitral valvulitis was mild and transient, although pancarditis was always accompanied by giant aneurysms, which determined an adverse prognosis.11
Among children with coronary lesions, 56% presented an incomplete form of the disease, an incidence similar to that described in the literature.4 In our population, male sex, age <27 months, prolonged fever, ESR>70 mm, and pancarditis were factors associated with coronary abnormalities.12
Generalized microvasculitis is expressed in 30%-50% of the patients as coronary ectasia. In all of these patients the condition resolved within the first 45 days of the disease. Coronary aneurysms can regress or progress. All aneurysms in group 2a involuted, compared with only 66% in group 2b. Giant aneurysms accounted for 15% of the total. These aneurysms do not involute, but can lead to obstruction.
Stress testing and myocardial perfusion (SPECT) images were used to detect myocardial ischemia.8 Coronary angiography should be performed7 if the patient is symptomatic or the noninvasive studies indicate myocardial ischemia, in order to assess feasibility of myocardial revascularization surgery,13 as occurred in 1 patient in our series.
CONCLUSIONS
Coronary aneurysms were the predominant cardiac lesions in our series. The risk factors for coronary aneurysms were age <27 months, prolonged fever of more than 8 days, ESR>70 mm, and pancarditis.
Correspondence:
Dra. A. M. Schroh.
Paso de los Andes, 812. Mendoza (5500). Argentina.
E-mail: schroh_md@hotmail.com
Received January 13, 2005.
Accepted for publication August 18, 2005.