Keywords
INTRODUCTION
The number of vascular procedures performed for diagnostic or therapeutic purposes has increased in recent years. Infectious vascular complications related with these procedures, such as bacteremia and local suppurating infection, are uncommon and often diagnosed late, a fact that increases the risk of an unfavorable clinical evolution due to bleeding or sepsis. We present our experience with 5 consecutive patients, whose clinical data are summarized in Table 1.
CLINICAL CASES
Case 1
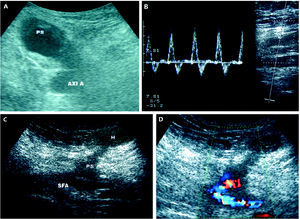
A 56-year-old man with a history of intermittent claudication. Arteriography showed severe atherosclerotic lesions in the infrarenal aorta and both iliac axes, which were treated with angioplasty and stent placement in both iliac arteries. Three months later the symptoms recurred. Arteriography was performed through the left axillary artery and a stent was placed in a restenosis of the left iliac artery. At 48 h following the procedure the axillary introducer was withdrawn, and 24 h later the patient presented with fever, pain and inflammation in the left axillary and pectoral region, with a bloody exudate from the puncture site. Culture of blood and exudate samples yielded Staphylococcus aureus. Echo-Doppler demonstrated a pseudoaneurysm in the axillary artery (Figure 1A). Cloxacillin treatment was started (2 g intravenously every 4 h) and maintained for 4 weeks prior to surgical resection of the pseudoaneurysm. Subsequently, oral ciprofloxacin (750 mg/12 h) and rifampicin (300 mg/12 h) were given for an additional 15 days. Later, the patient received oral ciprofloxacin treatment, with favorable evolution over the follow-up.
Figure 1. A: Ultrasound image of the pseudoaneurysm dependent on the left axillary artery in Case 1. B: Pulsed Doppler systolic-diastolic flow with the sample volume in the neck of the femoral pseudoaneurysm in Case 2. C: Pseudoaneurysm with a narrow neck, dependent on the superficial femoral artery, with an associated hematoma in Case 4. D: Color-Doppler image of panel C showing turbulent flow in the neck of the pseudoaneurysm. SFA indicates superficial femoral artery; AXI A, axillary artery; H, hematoma; PS, pseudoaneurysm
Case 2
A 40-year-old man with a history of smoking and type 2 diabetes mellitus. Elective percutaneous revascularization was performed following an inferior acute myocardial infarction (AMI) without fibrinolysis. The right femoral artery introducer was withdrawn by manual compression at 8 hours after the procedure. During the postoperative evolution, an inguinal mass appeared, corresponding to a pseudoaneurysm in the common femoral artery, which was resolved by local thrombin injection under ultrasound (US) guidance. Three months later the patient experienced a new episode of angina. Coronary angiography was performed through the left femoral artery, which showed no alterations. The artery was sutured with Perclose®. Twelve days later the patient developed fever, with pain, tumefaction and an inguinal hematoma. Serial blood cultures isolated methicillin-sensitive S aureus. Echo-Doppler and computed tomography (CT) examinations showed a heterogeneous collection adjacent to the left femoral artery. A few days later, a new echo-Doppler study disclosed a small, partially thrombosed pseudoaneurysm (Figure 1B). The patient's condition resolved completely after 7 days of intravenous vancomycin treatment (1 g/12 h) followed by a two-week course of oral ciprofloxacin (750 mg/12 h) associated with oral rifampicin (300 mg/ 12 h).
Case 3
A 61-year-old man with hypertension underwent coronary angiography and percutaneous revascularization through a right femoral access. The arterial introducer was withdrawn by manual compression 10 h after the procedure. Subsequently, a femoral artery pseudoaneurysm was detected and treated by US-guided percutaneous closure with thrombin. Twenty-five days following the procedure, the patient was hospitalized for fever with negative blood cultures and signs of inflammation in the right inguinal region. Recurrence of the aneurysm was confirmed by echo-Doppler and CT and the patient was treated with resection and surgical drainage. Culture of the surgical material yielded methicillin-sensitive S aureus and Escherichia coli. The patient was administered intravenous amoxicillin-clavulanic acid for 4 weeks with a favorable evolution.
Case 4
A 58-year-old man with a history of psoriatic arthritis, diabetes mellitus, arterial hypertension, and Buerger disease underwent arteriography of the lower limbs through the right femoral artery with an interventional procedure and arterial suture with Perclose®. He was readmitted at 15 days for a painful, pulsatile inguinal mass, and fever. Suspected pseudoaneurysm was confirmed by echo-Doppler (Figures 1C and D) and treated with a compression bandage. Three days later the patient was urgently operated because of massive bleeding in the same region. Fever reappeared three days later. Methicillin-sensitive S aureus was isolated in serial blood cultures and culture of the surgically removed tissue. Despite intravenous cloxacillin therapy (2 g/4 h) for 3 weeks, followed by oral levofloxacin (500 mg/24 h) and rifampicin (300 mg/12 h) for 1 additional week, persistent local infection was suspected; hence an endoprosthesis was implanted using a percutaneous approach to isolate the femoral artery.
Case 5
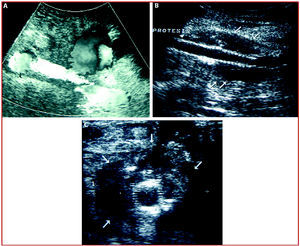
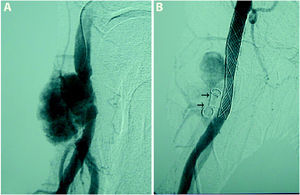
A 68-year-old man with a history of smoking and poorly controlled hypertension. A stent was implanted in the left renal artery and the right femoral access was sutured with Perclose®. One month later, the patient was readmitted for a hematoma and signs of inflammation in the right inguinal region. Echo-Doppler confirmed a suspected pseudoaneurysm (Figure 2A), which was surgically resected. In the immediate postoperative period, fever and a pulsatile mass developed, consistent with local recurrence. Empirical treatment with intravenous cloxacillin (2 g/4 h) was decided and the right femoral artery was isolated by implantation of an endoprosthesis. In addition, the deep femoral artery was embolized with coils after confirming its involvement in the pseudoaneurysm (Figure 3A and B). Local infection persisted and echo-Doppler demonstrated a periprosthetic collection (Figures 2B and C). The patient underwent surgical drainage and removal of the abscessed hematoma with a second attempt at closure. Antibiotic treatment with cloxacillin was given for 3 weeks followed by oral levofloxacin (500 mg/24 h) plus oral rifampicin (300 mg/12 h) for 1 additional week. Culture of the resected material yielded S aureus.
Figure 2. A: Color echo-Doppler of Case 5 showing "swirling" flow within the pseudoaneurysm. B: Case 5, longitudinal section. The femoral endoprosthesis (arrowhead) with a periprosthetic collection (arrows) is evident. C: Case 5, transversal section of panel B. Periprosthetic collection (arrows).
Figure 3. A: Arteriography of Case 5. Pseudoaneurysm in the right superficial femoral artery. B: Case 5. The aneurysm has disappeared following percutaneous placement of a femoral endoprosthesis. Coils in the deep femoral artery (arrows).
DISCUSSION
Postcatheterization infectious vascular complications are uncommon (<1%) and most of the reported cases involve bacteremia.1 The series presented includes local vascular infections, which accounted for 0.1% of the total of catheterization procedures performed in our center during July 2000 to June 2004. The main challenge inherent to these cases is differentiating between infected hematomas (which secondarily affect the artery by contiguity) and arteritis with formation of pseudoaneurysms and soft tissue abscesses with associated superficial cellulitis. Clinical risk factors have been reported for this complication, such as the presence of heart failure, and factors related to the procedure (difficult access, repeated puncture, and prolonged catheter insertion),2 although this last point is more controversial.3,4 In our series, both manual compression and the Perclose® system were used for arterial closure (Table); nevertheless, it seems reasonable to consider a possible relationship between suturing and local contamination, since it has been reported that the use of arterial closure systems can increase the risk of local infection (0.3%-0.4% incidence) as compared to manual compression.5,6
In Case 3 percutaneous closure of a pseudoaneurysm with thrombin was undertaken. Although it is difficult to demonstrate a causal association,7 the technique requires manipulation of the area with the ultrasound probe and sometimes, several punctures, which would undoubtedly be a potential source of contamination from the epidermis. This justifies taking utmost precautions (e.g., isolation of the sonographic probe with latex gloves and adequate asepsis) when using these techniques to close pseudoaneurysms.
In most cases the infection manifests early with fever and local symptoms, but the diagnosis is often delayed because clinical suspicion is low and the condition can be mistaken for hematomas or superficial ecchymosis. As occurred in our series, many patients experience bacteremia and the most frequently isolated microorganism is S aureus8; hence blood cultures and empirical treatment with antibiotics active against this microorganism are mandatory.
Echo-Doppler proved to be very helpful in our series to establish the diagnosis of local complications, although serial examinations are sometimes needed to confirm the findings. Surgical treatment seems necessary to drain abscesses and hematomas, and to remove pseudoaneurysms9; nonetheless, in very early cases and when there is severe vascular compromise in seriously ill patients at high surgical risk, implantation of an endoprosthesis can be a good alternative.10
It is expected that in the coming years the number of these severe infections in percutaneous vascular procedures will increase, a fact that should be kept in mind when managing patients who show post-procedure fever and signs of inflammation at the puncture site. Blood culture and examination with imaging techniques such as echo-Doppler will allow an early diagnosis to be established and improve the prognosis. It is likely that the growing use of radial accesses will decrease the number of these complications and modify their treatment.11
Correspondence:
Dr. M. Almendro Delia.
Servicio de Cardiología. Hospital Universitario Virgen Macarena.
Sevilla, 37. 41410 Carmona. Sevilla. España.
E-mail: trocor@yahoo.es
Received April 12, 2005.
Accepted for publication August 19, 2005.