Recently, substantial discrepancies have been detected between clinical guideline recommendations and the actual treatment prescribed1 to patients with ischemic heart disease (IHD) or atrial fibrillation (AF). In this study, we assessed the impact of a change from a classic model of care coordination between primary care (PC) and cardiology to a more integrated model in the region covered by Hospital Moisès Broggi (Barcelona, Spain), on target low-density lipoprotein cholesterol (LDL-C) levels in patients with IHD and on the degree of anticoagulation in patients with AF.
This was an ecological study of aggregate data by center, which involved a retrospective analysis of the characteristics of the patients who received care at the centers where the new integrated model was implemented (426 377 patients; 19 PC centers) and those who received care at centers where the classic model (105 936 patients; 6 PC centers) at one time point before (2013) and one time point after (2017) the introduction of the integrated care model. In the classic model, the patients are seen by a cardiologist in the hospital outpatient cardiology clinic, for their first and subsequent follow-up visits. In the integrated model, a cardiologist goes once a week to the PC centers, where they hold in-person or virtual consultations and joint sessions (our group has analyzed these data in a study that is pending publication).
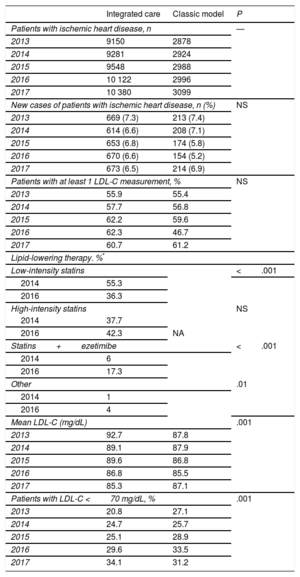
At the study start, 32.0% and 32.5% of the patients with IHD in the integrated care and classic care models, respectively, were women. The mean age was 72.7±11.6 and 71.8±12.1 years. In the areas where the new model was implemented, there was a higher intensity of lipid-lowering therapy, and the mean LDL-C value decreased (from 92.7 to 85.3mg/dL) significantly compared with the classic group (87.8 to 87.1mg/dL). This translated to a higher percentage of LDL-C target levels being met (from 20.8% to 34.1% [relative increase of 63.9%] and from 27.1% to 31.2% [relative increase of 15.1%]; P <0.001) (Table 1).
Incidence/prevalence and Lipid Parameters of Patients With Chronic Ischemic Heart Disease According to Care Model
| Integrated care | Classic model | P | |
|---|---|---|---|
| Patients with ischemic heart disease, n | — | ||
| 2013 | 9150 | 2878 | |
| 2014 | 9281 | 2924 | |
| 2015 | 9548 | 2988 | |
| 2016 | 10 122 | 2996 | |
| 2017 | 10 380 | 3099 | |
| New cases of patients with ischemic heart disease, n (%) | NS | ||
| 2013 | 669 (7.3) | 213 (7.4) | |
| 2014 | 614 (6.6) | 208 (7.1) | |
| 2015 | 653 (6.8) | 174 (5.8) | |
| 2016 | 670 (6.6) | 154 (5.2) | |
| 2017 | 673 (6.5) | 214 (6.9) | |
| Patients with at least 1 LDL-C measurement, % | NS | ||
| 2013 | 55.9 | 55.4 | |
| 2014 | 57.7 | 56.8 | |
| 2015 | 62.2 | 59.6 | |
| 2016 | 62.3 | 46.7 | |
| 2017 | 60.7 | 61.2 | |
| Lipid-lowering therapy. %* | |||
| Low-intensity statins | <.001 | ||
| 2014 | 55.3 | ||
| 2016 | 36.3 | ||
| High-intensity statins | NS | ||
| 2014 | 37.7 | ||
| 2016 | 42.3 | NA | |
| Statins+ezetimibe | <.001 | ||
| 2014 | 6 | ||
| 2016 | 17.3 | ||
| Other | .01 | ||
| 2014 | 1 | ||
| 2016 | 4 | ||
| Mean LDL-C (mg/dL) | .001 | ||
| 2013 | 92.7 | 87.8 | |
| 2014 | 89.1 | 87.9 | |
| 2015 | 89.6 | 86.8 | |
| 2016 | 86.8 | 85.5 | |
| 2017 | 85.3 | 87.1 | |
| Patients with LDL-C <70 mg/dL, % | .001 | ||
| 2013 | 20.8 | 27.1 | |
| 2014 | 24.7 | 25.7 | |
| 2015 | 25.1 | 28.9 | |
| 2016 | 29.6 | 33.5 | |
| 2017 | 34.1 | 31.2 | |
LDL-C, low density lipoprotein cholesterol; NA, not available; NS, not significant.
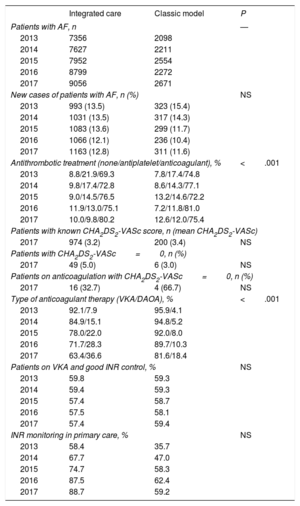
At baseline, 50.9% and 54.3% of the patients with AF were women, and the mean age was 80.3±10.5 and 79.2±11.1 years. In the integrated care centers, the percentage of patients on anticoagulant therapy increased significantly (from 69.3% to 80.2% [relative increase of 15.7%]; P <0.001), unlike in the classic model (from 74.8% to 75.4% [relative increase of 0.8%]; P=NS; P <0.001 between groups). Similarly, while there was a marked decrease in use of antiplatelets in the integrated model group, in the classic model this reduction was smaller (relative decrease of 55.3% vs 31.0%; P <0.001). Although the prescription of direct-acting anticoagulants increased in both groups, the increase was larger in the patients receiving care under the new model (from 7.9% to 36.6% and 4.1% to 18.4%; P <0.001). Both groups had a similar increase in international normalized ratio (INR) monitoring carried out in PC, with no differences regarding good INR control, defined as time in therapeutic range ≥ 60%. No significant differences were found between the 2 groups in the CHA2DS2-VASc score (Table 2).
Incidence/prevalence of AF and Antithrombotic treatment According to Çare Model
| Integrated care | Classic model | P | |
|---|---|---|---|
| Patients with AF, n | — | ||
| 2013 | 7356 | 2098 | |
| 2014 | 7627 | 2211 | |
| 2015 | 7952 | 2554 | |
| 2016 | 8799 | 2272 | |
| 2017 | 9056 | 2671 | |
| New cases of patients with AF, n (%) | NS | ||
| 2013 | 993 (13.5) | 323 (15.4) | |
| 2014 | 1031 (13.5) | 317 (14.3) | |
| 2015 | 1083 (13.6) | 299 (11.7) | |
| 2016 | 1066 (12.1) | 236 (10.4) | |
| 2017 | 1163 (12.8) | 311 (11.6) | |
| Antithrombotic treatment (none/antiplatelet/anticoagulant), % | <.001 | ||
| 2013 | 8.8/21.9/69.3 | 7.8/17.4/74.8 | |
| 2014 | 9.8/17.4/72.8 | 8.6/14.3/77.1 | |
| 2015 | 9.0/14.5/76.5 | 13.2/14.6/72.2 | |
| 2016 | 11.9/13.0/75.1 | 7.2/11.8/81.0 | |
| 2017 | 10.0/9.8/80.2 | 12.6/12.0/75.4 | |
| Patients with known CHA2DS2-VASc score, n (mean CHA2DS2-VASc) | |||
| 2017 | 974 (3.2) | 200 (3.4) | NS |
| Patients with CHA2DS2-VASc=0, n (%) | |||
| 2017 | 49 (5.0) | 6 (3.0) | NS |
| Patients on anticoagulation with CHA2DS2-VASc=0, n (%) | |||
| 2017 | 16 (32.7) | 4 (66.7) | NS |
| Type of anticoagulant therapy (VKA/DAOA), % | <.001 | ||
| 2013 | 92.1/7.9 | 95.9/4.1 | |
| 2014 | 84.9/15.1 | 94.8/5.2 | |
| 2015 | 78.0/22.0 | 92.0/8.0 | |
| 2016 | 71.7/28.3 | 89.7/10.3 | |
| 2017 | 63.4/36.6 | 81.6/18.4 | |
| Patients on VKA and good INR control, % | NS | ||
| 2013 | 59.8 | 59.3 | |
| 2014 | 59.4 | 59.3 | |
| 2015 | 57.4 | 58.7 | |
| 2016 | 57.5 | 58.1 | |
| 2017 | 57.4 | 59.4 | |
| INR monitoring in primary care, % | NS | ||
| 2013 | 58.4 | 35.7 | |
| 2014 | 67.7 | 47.0 | |
| 2015 | 74.7 | 58.3 | |
| 2016 | 87.5 | 62.4 | |
| 2017 | 88.7 | 59.2 | |
AF, atrial fibrillation; DAOA, direct-acting oral anticoagulants; INR, international normalized ratio; VKA, vitamin K antagonist.
While LDL-C control has improved over the past decade in Spain, more than 70% of patients on secondary prevention still do not meet target levels, suggesting that, despite treatment intensification, treatment is insufficient.2 Our results show that there was a similar increase in the 2 groups in the number of LDL-C measurements, which would suggest a greater awareness of achieving LDL-C targets. However, the integrated model was associated with a higher intensity of lipid-lowering therapy (greater use of high-potency statins and above all combined treatment), which would explain the greater reduction in LDL-C and consequently the higher proportion of patients meeting targets. Thus, an integrated care model can help to improve LDL-C control in secondary prevention. Unfortunately, the figures are still very poor,2 indicating that greater effort is needed.
Most patients with AF should be on anticoagulant therapy. However, previous studies have shown that up to one-third of patients at high risk are not anticoagulated in practice,3 a figure that is similar to that found in 2013 in both groups. Our data indicate that, although there is still a percentage of patients that are not on anticoagulation, integrated care could substantially reduce these levels. Approximately 40% to 45% of the patients had poor INR control, independently of the type of care received, a finding similar to previously-reported figures,4 suggesting that additional measures are required. Direct-acting anticoagulants are particularly indicated for patients with poor INR control. In Spain they are clearly underused. Our data suggest that the integrated care model could help to detect these patients and optimize the prescription of these anticoagulants.
In conclusion, our data show that PC-cardiology integrated care can improve LDL-C control in secondary prevention and optimize anticoagulant therapy in patients with AF, which could ultimately improve health outcomes.
The authors thank the Cardiology-Primary Care Integrated Care working group for the Hospital Moisès Broggi region.
Content Ed Net, Madrid, provided editorial assistance in writing this article.